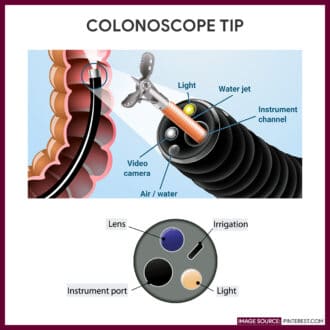
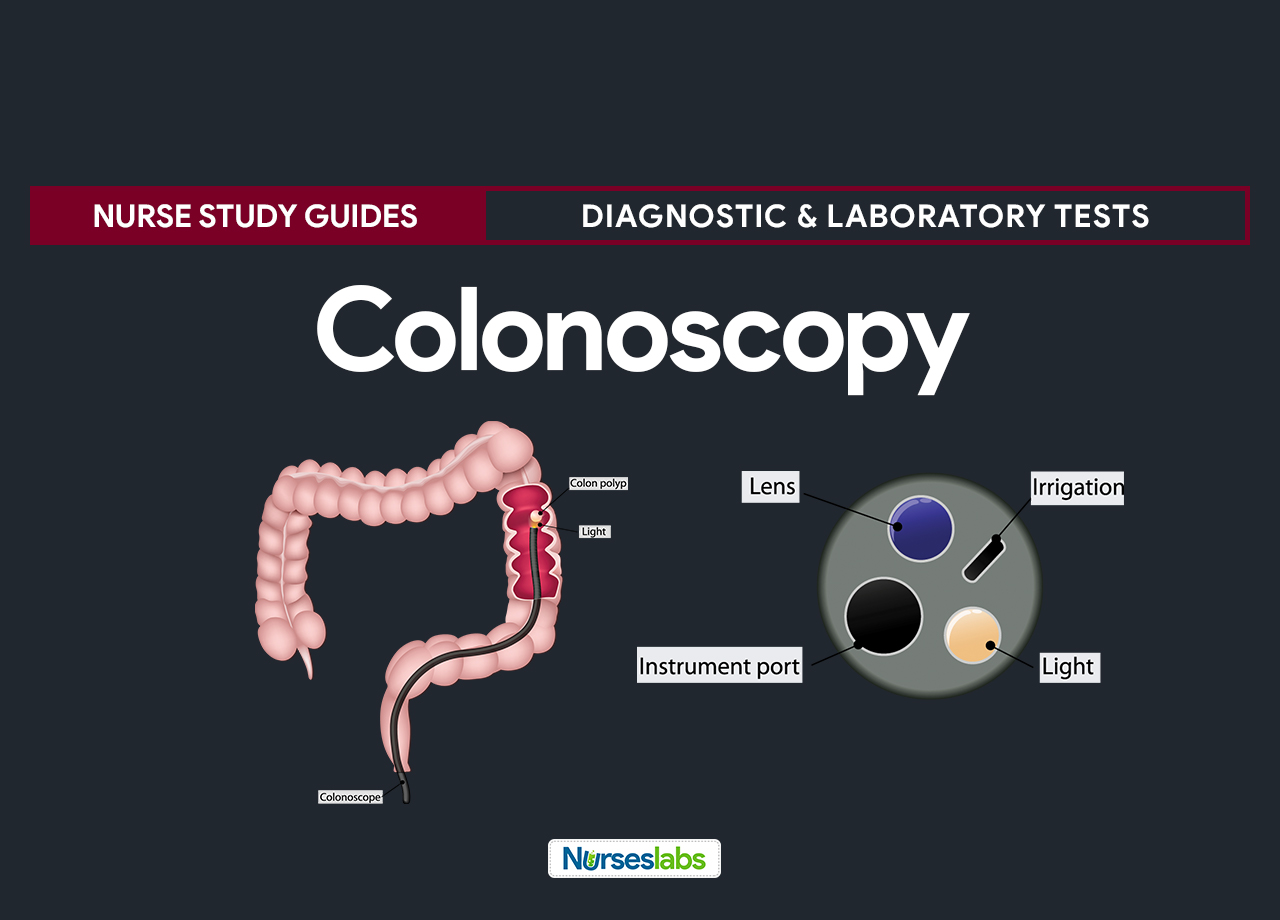
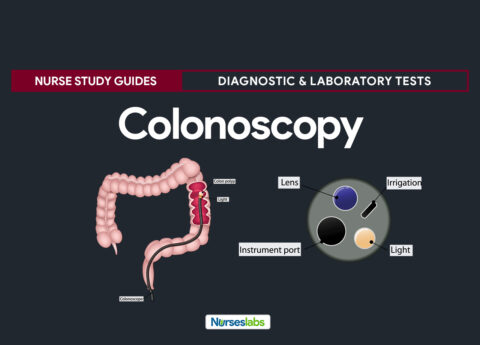
Colonoscopy is a diagnostic procedure that utilizes a flexible fiberoptic colonoscope inserted into the rectum to examine the large intestine (colon) lining visually. It is indicated for patients with a history of constipation, diarrhea, persistent rectal bleeding, and lower abdominal pain when the results of proctosigmoidoscopy and a barium enema test are negative or inconclusive.
The nurse’s responsibility during colonoscopy encompasses different tasks to ensure the patient’s safety before, during, and after the procedure. It is also the nurse’s responsibility to bowel prep the patient for colonoscopy, obtain informed consent and ease the patient’s anxiety by providing information about the procedure.
Aside from assisting the physician during the colonoscopy, another essential task of the nurse is to ensure patient safety when the colonoscope is reprocessed. Proper cleaning, disinfection, and sterilization of the equipment is an important step to prevent infection from patient to patient. Proper reprocessing involves wiping the scope tube with a lint-free cloth soaked using a detergent solution, then taking it to a sterile reprocessing room for meticulous cleaning, leak testing, visual examination, and sterilizing.
This study guide can help nurses understand their tasks and responsibilities during colonoscopy.
Colonoscopy Indication
Colonoscopy is indicated for several reasons, which includes:
- Screen for colon and rectal cancer
- Detect and evaluate inflammatory and ulcerative bowel disease
- Locate the source of lower GI bleeding and perform hemostasis by coagulation
- Determine the cause of lower GI disorders, especially when barium and proctosigmoidoscopy results are inconclusive
- Assist diagnose colonic strictures and benign or malignant lesions
- Evaluate the colon postoperatively for recurrence of polyps and malignant lesions
- Investigate iron-deficiency anemia of unknown origin
- Remove colon polyps
- Remove foreign objects and sclerosing strictures by laser
Contraindication
This procedure is contraindicated for:
- Pregnant women near term
- Patients with bleeding disorders
- Patients who had a recent acute myocardial infarction or abdominal surgery
- Patients with ischemic bowel disease, acute diverticulitis, peritonitis, fulminant granulomatous colitis, perforated viscus, or fulminant ulcerative colitis: For these cases or for screening purposes, virtual colonoscopy may help visualize polyps before they become concerns.
Procedure
Steps to colonoscopy are performed as follows:
- The patient is placed on his left side with his knees flexed and draped.
- Baseline vital signs are obtained. Vital signs are monitored throughout the procedure. If the patient has known cardiac disease, continuous electrocardiographic monitoring should be instituted. Continuous or periodic pulse oximetry is advisable, particularly in the high-risk patient with possible respiratory depression secondary to sedation, which may be given.
- The patient is instructed to breathe deeply and slowly through his mouth as the practitioner palpates the mucosa of the anus and rectum and inserts, under direct vision, the lubricated colonoscope through the patient’s anus into the sigmoid colon.
- A small amount of air is insufflated to locate the bowel lumen, and then the scope is advanced through the rectum.
- When the instrument reaches the descending sigmoid junction, the patient is assisted to a supine position to aid the scope advance, if necessary. After passing the splenic flexure, the scope is advanced through the transverse colon, through the hepatic flexure, and into the ascending colon and cecum.
- Abdominal palpation or fluoroscopy may be used to help guide the colonoscope through the large intestine.
- Suction may be used to remove blood and secretions that obscure the vision.
- Biopsy forceps or a cytology brush may be passed through the colonoscope to obtain specimens for histologic or cytologic examination; an electrocautery snare may be used to remove polyps.
- If the physician removes a tissue specimen, it’s placed immediately in a specimen bottle containing 10% formalin; cytology smears are immediately placed in a Coplin jar containing 95% ethyl alcohol. Specimens are sent to the laboratory immediately.
Interfering factors
These are factors that may affect the outcome of the colonoscopy:
- Insufficient bowel preparation or failure to restrict food intake prior to the procedure
- Retained barium in the intestine from previous diagnostic procedure
- Inability of the patient to tolerate introduction of or retention of barium, air, or both in the bowel
- Sigmoid colon fixation due to inflammatory bowel disease, surgery, or radiation therapy that may hinder the passage of the colonoscope
- Blood from acute colonic hemorrhage which can interfere with visualization
- Colon spasms which can mimic the radiographic signs of cancer
Nursing Responsibilities
The following are the nursing interventions and nursing care considerations for the patient:
Before the procedure
The following are the nursing interventions before colonoscopy:
- Secure an informed consent. Make sure that the patient or a significant other has signed an informed consent form.
- Obtain a medical history of the patient. Check for allergies, bleeding histories, medications, and information relevant to the current complaint.
- Provide information about the procedure. Tell the patient that colonoscopy permits examination of the large intestine’s lining. Describe the procedure and tell the patient who will perform it and where it will take place.
- Ensure that the patient has complied with the bowel preparation. Explain that the large intestine must be thoroughly cleaned to be clearly visible. To do so, tell the patient that he must maintain a clear-liquid diet for 24 to 48 hours before the test, take nothing by mouth after midnight the before, and take a laxative, as ordered, or 1 gallon of GoLYTELY solution in the evening (drinking the chilled solutions at 8 oz [236.6 ml] every 10 minutes until the entire gallon is consumed).
- Establish an IV line. Inform the patient that an IV line will be started and a sedative will be administered before the procedure. Because a sedative will be given, advise the patient to arrange for someone to drive him home after the procedure.
- Provide reassurance. Assure the patient that the colonoscope is well lubricated to ease it’s insertion, that it initially feels cool, and that he may feel an urge to defecate when it’s inserted and advanced.
- Explain to the patient that air may be introduced through the colonoscope. This is done to distend the intestinal wall and to facilitate viewing the lining and advancing the instrument. Tell him that flatus normally escapes around the instrument because of air insufflation and that he shouldn’t attempt to control it.
- Instruct the patient to empty bladder prior to the procedure. It is more comfortable if the patient voids immediately before the procedure and to change into the gown, robe, and foot coverings provided.
- Instruct the patient to remove all metallic objects from the area to be examined. Metallic objects such as jewelry within the examination area may alter organ visualization and cause unclear images.
- Instruct the patient to cooperate and follow directions. Instruct patient to remain still during the procedure because movement creates unreliable results.
During the procedure
The following are the nursing interventions during colonoscopy:
- Assist with patient positioning as necessary. Place the patient on the examination table in a left lateral decubitus position with a sheet draped over the body.
- Administer medications as ordered. Pain medication and sedative will be given to reduce discomfort and to promote relaxation.
- Instruct the patient to bear down. Bearing down as if having a bowel movement is advised as the fiberoptic tube is inserted through the rectum.
- Change the position of the patient. When the scope is advanced through the sigmoid. The patient’s position is changed to supine to allow passage into the transverse colon. Air is insufflated through the tube during the passage to help in visualization.
- Encourage the patient to take slow, deep breaths. Instruct the patient to take deep breaths to aid in the movement of the scope down through the ascending colon to the cecum and into the terminal portion of the ileum.
After the procedure
The nurse should note the following nursing interventions post-colonoscopy:
- Observe the patient closely for signs of bowel perforation. Signs of bowel perforations such as severe abdominal pain, nausea, vomiting, fever, and chills must be reported immediately.
- Obtain and record the patient’s vital signs. Monitor vital signs and neurological status every 15 minutes for 1 hour, then every 2 hours for 4 hours, or as ordered. Assess temperature every 4 hours for 24 hours.
- Instruct patient to resume a normal diet, fluids, and activity as advised by the health care provider. After the patient has recovered from sedation, allow him to resume his usual diet and activity unless the practitioner orders otherwise.
- Provide privacy while the patient rest after the procedure. Inform that the patient may pass large amounts of flatus after insufflation.
- Monitor for any rectal bleeding. If a polyp has been removed, minimal rectal bleeding is expected for 2 days but an increasing amount of bleeding should be reported immediately.
- Encourage increased fluid intake. Fluids must be given to replace fluid lost during the preparation of the procedure.
Normal results
Normal findings of colonoscopy will show a:
- Light-pink-orange mucosa of the large intestine beyond the sigmoid colon that is marked by semilunar folds and deep tubular pits.
- Visible blood vessels beneath the intestinal mucosa, which glisten from mucus secretions.
Abnormal results
Abnormal colonoscopy findings may reveal:
- Benign or malignant lesions
- Bowel inflammation and ulceration
- Granulomatous or ulcerative colitis
- Colonic polyps
- Crohn’s disease
- Diverticular disease or the site of lower GI bleeding.
- Hemorrhoids
- Proctitis
- Tumors
- Vascular abnormalities
Gallery
Images related to colonoscopy:


References
Additional resources and references for the colonoscopy study guide:
- Colorectal Cancer Early Detection, Diagnosis, and Staging. (2018). Retrieved from https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging.html
- Rex, D. K., Petrini, J. L., Baron, T. H., Chak, A., Cohen, J., Deal, S. E., … & Safdi, M. A. (2006). Quality indicators for colonoscopy. Gastrointestinal Endoscopy, 63(4), S16-S28.
- Lieberman, D. A., Weiss, D. G., Bond, J. H., Ahnen, D. J., Garewal, H., Harford, W. V., … & Nelson, D. B. (2000). Use of colonoscopy to screen asymptomatic adults for colorectal cancer. New England Journal of Medicine, 343(3), 162-168.
- Waye, J. D., Lewis, B. S., & Yessayan, S. (1992). Colonoscopy: a prospective report of complications. Journal of clinical gastroenterology, 15(4), 347-351.















Leave a Comment