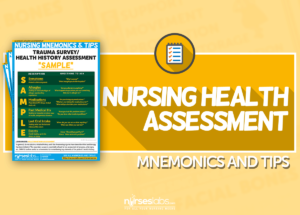
They say that the best nurses are excellent at obtaining assessment, and this is true! If nurses would look at the nursing process, assessment is the first and key step.
Gathering information about the client will provide clues for what care you can give and what you can intervene. If you have a weak foundation in assessment, the rest of the process follows.
But with the many ways to assess a patient, assessment has become an overwhelming process. To be more systematic, here are nursing health assessment mnemonics & tips you can use to accurately and quickly assess variety of patients in with different conditions and in various situations.
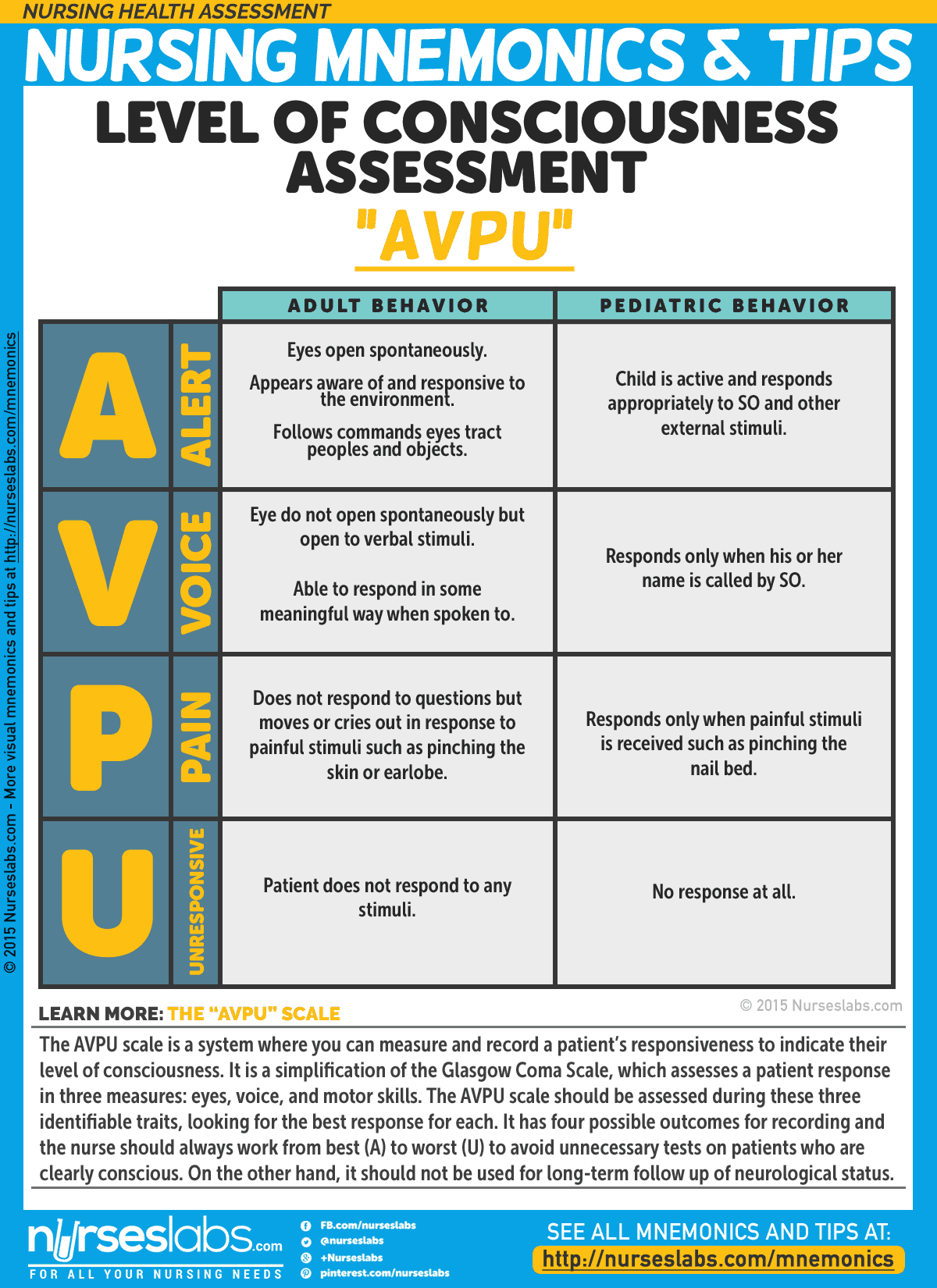
1. Level of Consciousness Assessment: “AVPU”
The AVPU scale is a system where you can measure and record a patient’s responsiveness to indicate their level of consciousness. It is a simplification of the Glasgow Coma Scale, which assesses a patient response in three measures: eyes, voice, and motor skills. The AVPU scale should be assessed during these three identifiable traits, looking for the best response for each. It has four possible outcomes for recording and the nurse should always work from best (A) to worst (U) to avoid unnecessary tests on patients who are clearly conscious. On the other hand, it should not be used for long-term follow up of neurological status.
- A: Alert
- V: Response to Verbal Stimuli
- P: Response to Pain
- U: Unresponsive
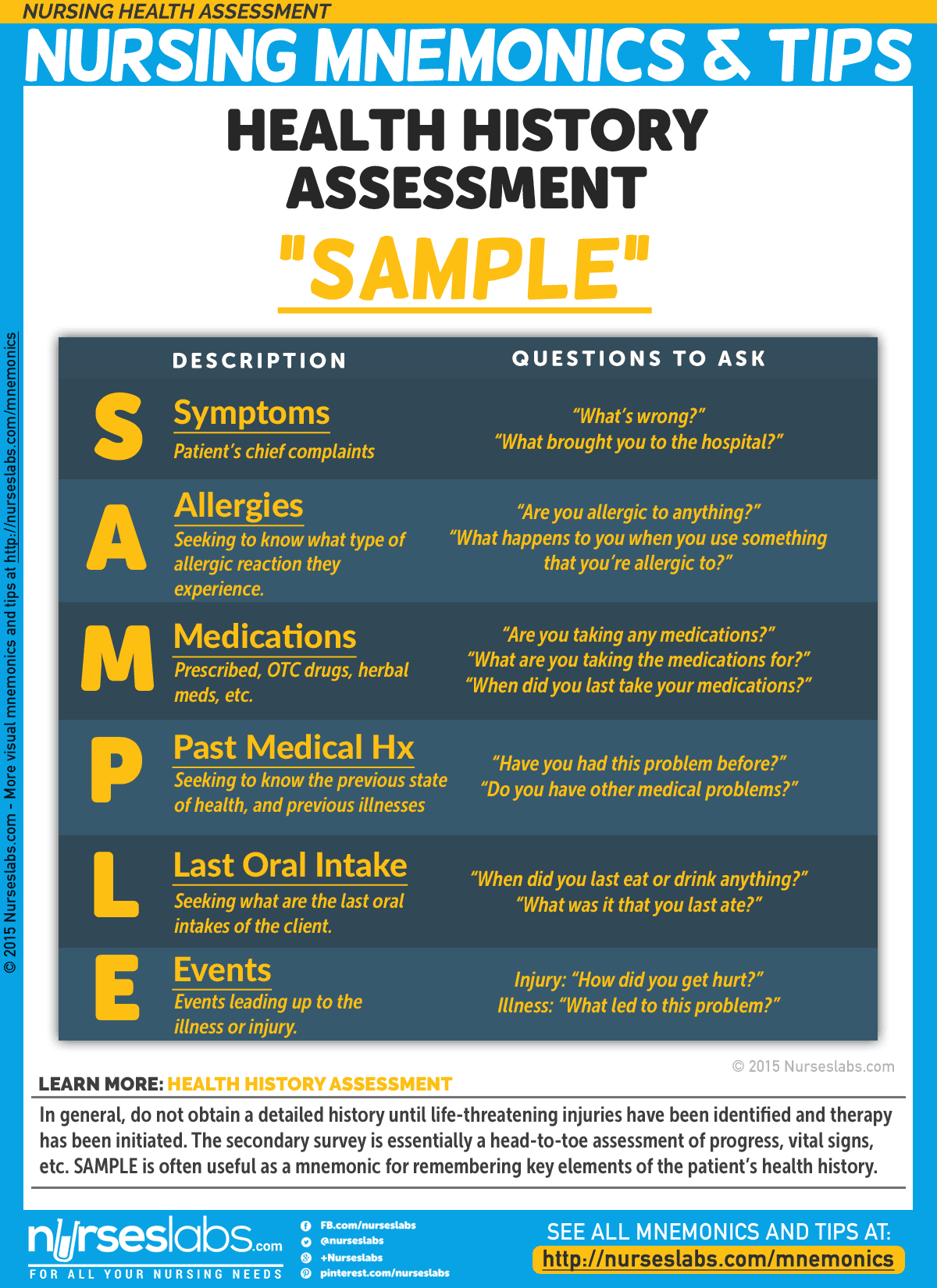
2. Health History Assessment: “SAMPLE”
In general, do not obtain a detailed history until life-threatening injuries have been identified and therapy has been initiated. The secondary survey is essentially a head-to-toe assessment of progress, vital signs, etc. SAMPLE is often useful as a mnemonic for remembering key elements of the patient’s health history.
- S: Symptoms
- A: Allergy
- M: Medications
- P: Past Medical History
- L: Last Oral Intake
- E: Events leading up to the illness or injury
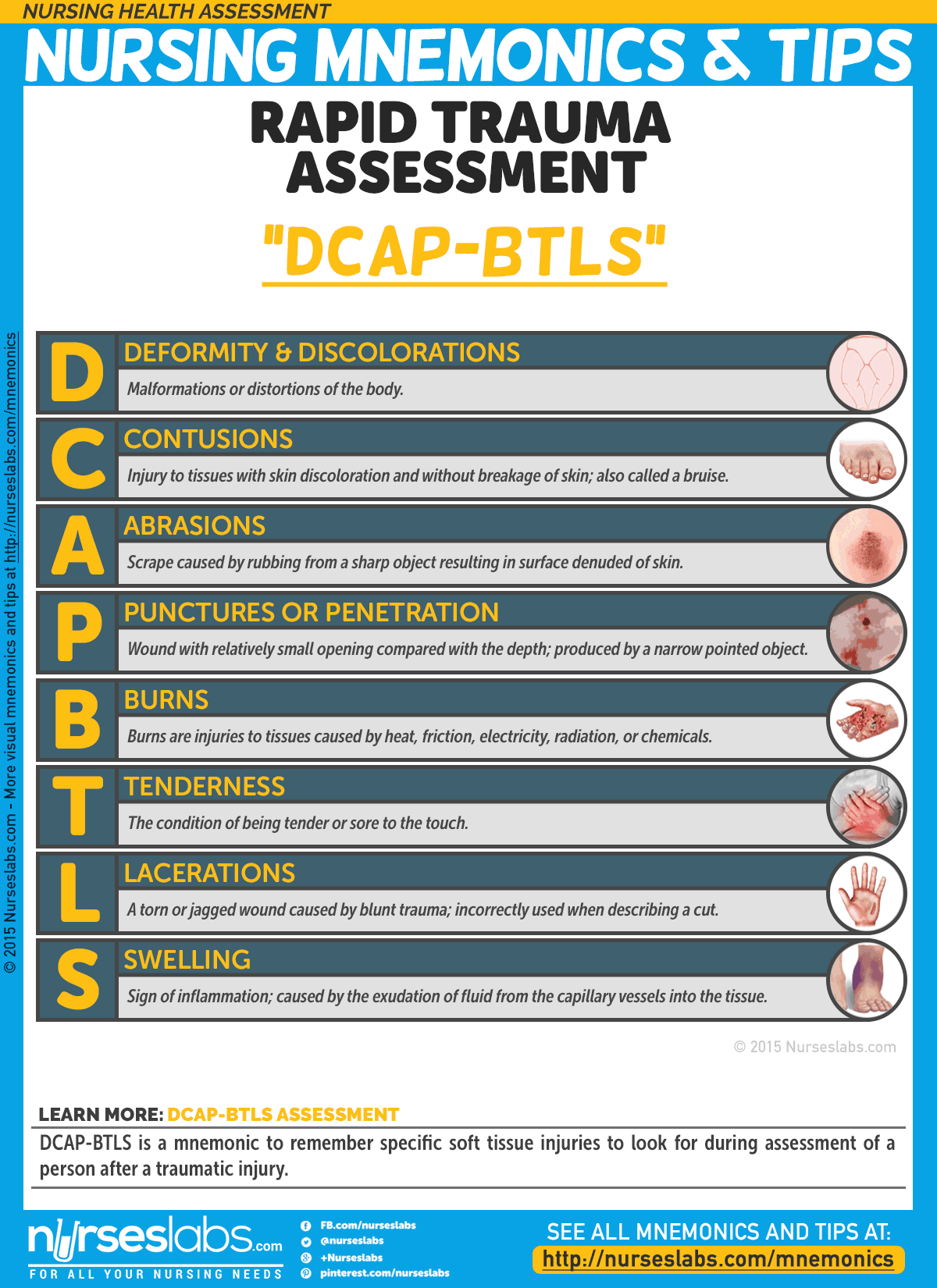
3. Rapid Trauma Assessment: “DCAP-BTLS”
DCAP-BTLS is a mnemonic to remember specific soft tissue injuries to look for during assessment of a person after a traumatic injury.
- D: Deformities
Malformations or distortions of the body. - C: Contusions
Injury to tissues with skin discoloration and without breakage of skin; also called a bruise. - A: Abrasions
Scrape caused by rubbing from a sharp object resulting in surface denuded of skin. - P: Punctures or Penetrations
Wound with relatively small opening compared with the depth; produced by a narrow pointed object. - B: Burns
Burns are injuries to tissues caused by heat, friction, electricity, radiation, or chemicals. - T: Tenderness
The condition of being tender or sore to the touch. - L: Lacerations
A torn or jagged wound caused by blunt trauma; incorrectly used when describing a cut. - S: Swelling
Sign of inflammation; caused by the exudation of fluid from the capillary vessels into the tissue.
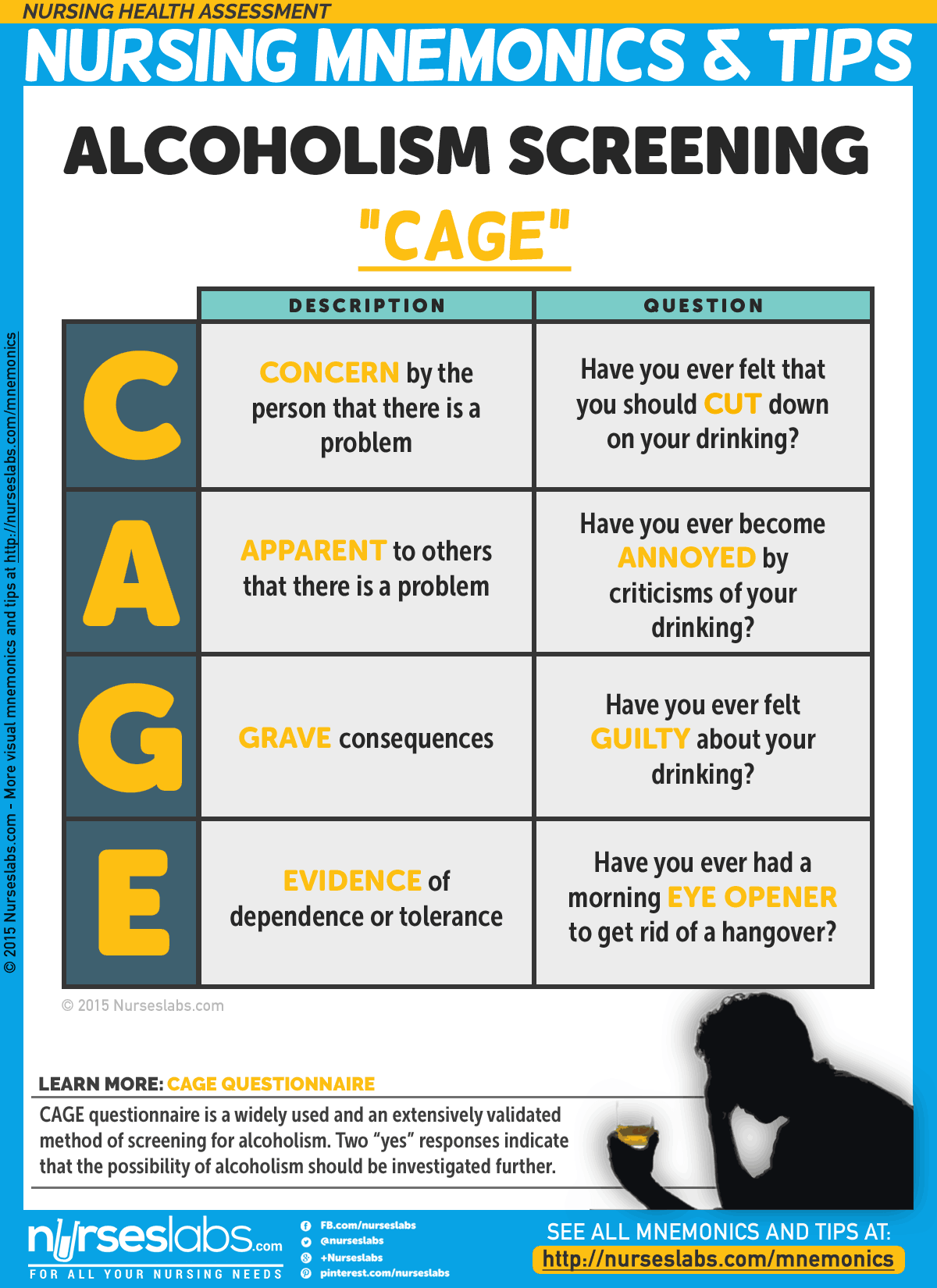
4. Alcoholism Screening: “CAGE”
CAGE questionnaire is a widely used and an extensively validated method of screening for alcoholism. Two “yes” responses indicate that the possibility of alcoholism should be investigated further. By far the most important question in the CAGE questionnaire is the use of a drink as an Eye Opener, so much so that some clinicians use a “yes” to this question alone as a positive to the questionnaire; this is because the use of an alcoholic drink as an Eye Opener connotes dependence since the patient is going through possible withdrawal in the morning, hence the need for a drink as an Eye Opener.
- C: Have you ever felt that you should CUT down on your drinking?
- A: Have you ever become ANNOYED by criticisms of your drinking?
- G: Have you ever felt GUILTY about your drinking?
- E: Have you ever had a morning EYE OPENER to get rid of a hangover?
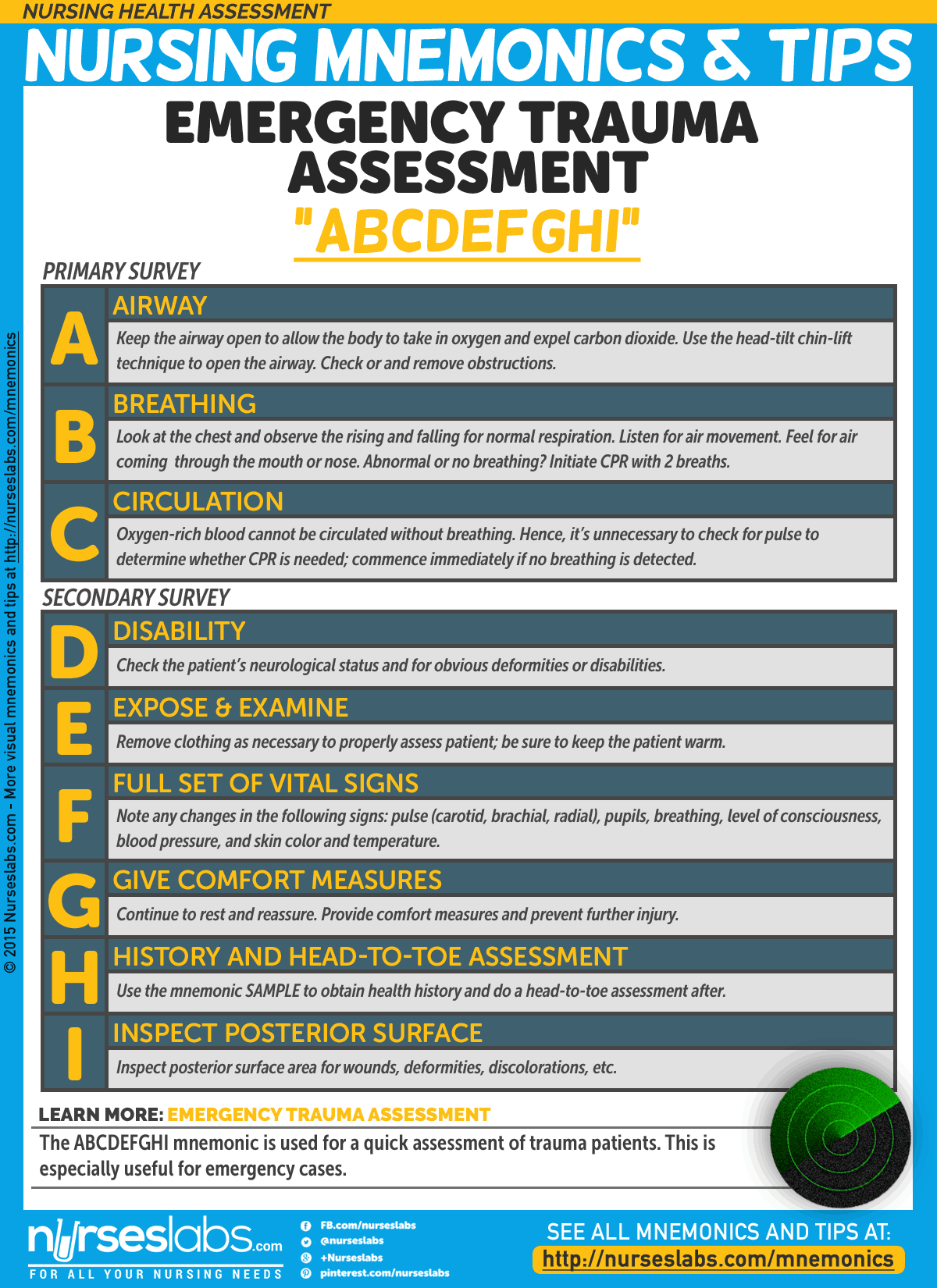
5. Emergency Trauma Assessment: “ABCDEFGHI”
The ABCDEFGHI mnemonic is used for a quick assessment of trauma patients. This is especially useful for emergency cases. The purpose of primary assessment is to preserve the life of the victim, taking action where needed. Once the victim’s life-threatening conditions have been address, the rescuer must begin secondary assessment.
- A: Airway
Keep the airway open to allow the body to take in oxygen and expel carbon dioxide. Use the head-tilt chin-lift technique to open the airway. Check or and remove obstructions. A blocked airway can lead to respiratory or cardiac arrest. - B: Breathing
Once the airway is open, check for normal breathing, make use of the look, listen, and feel techniques.
Look at the chest and observe the rising and falling for normal respiration. Listen for air movement. Feel for air coming through the mouth or nose. If there is no breathing or abnormal breathing, CPR must be initiated with 2 breaths. - C: Circulation
Oxygen-rich blood cannot be circulated without breathing. Hence, it’s unnecessary to check for pulse to determine whether CPR is needed; commence immediately if no breathing is detected. - D: Disability
Check the patient’s neurological status and for obvious deformities or disabilities. - E: Expose & Examine
Remove clothing to properly assess patient; be sure to keep the patient warm. - F: Full set of vital signs
Note any changes in the following signs: pulse (carotid, brachial, radial), pupils, breathing, level of consciousness, blood pressure, and skin color and temperature. - G: Give comfort measures
Continue to rest and reassure. Provide comfort measures and prevent further injury. - H: History and Head-To-Toe Assessment
Use the mnemonic SAMPLE to obtain health history and do a head-to-toe assessment after. - I: Inspect Posterior Surface
Inspect for wounds, deformities, discolorations, etc.
6. Seven Warning Signs of Cancer: “CAUTION”
Early detection is the key in treatment of cancers. The CAUTION mnemonic is used by the American Cancer Society to detect and recognize the early warning signs of cancer. Though one of these signs does not necessarily mean someone has cancer.
- C: Change in bowel or bladder habits
- A: A sore throat that does not heal
- U: Unusual bleeding or discharge
- T: Thickening or lump in breast or elsewhere
- I: Indigestion or dysphagia
- O: Obvious change in wart or mole
- N: Nagging cough or hoarseness
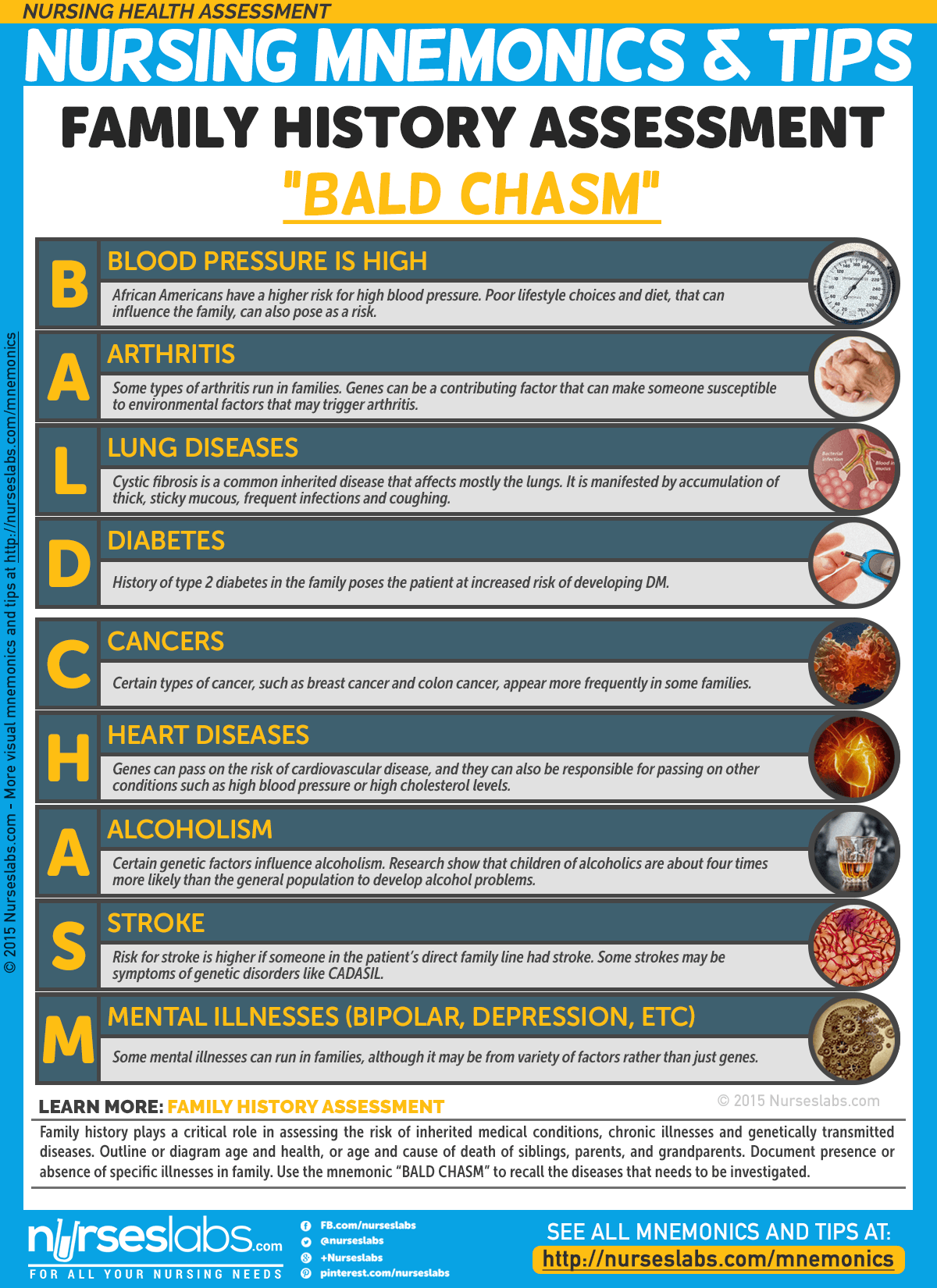
7. Family History Assessment: “BALD CHASM”
Family history plays a critical role in assessing the risk of inherited medical conditions, chronic illnesses and genetically transmitted diseases. Outline or diagram age and health, or age and cause of death of siblings, parents, and grandparents. Document presence or absence of specific illnesses in family. Use the mnemonic “BALD CHASM” to recall the diseases that needs to be investigated.
- B: Blood pressure
African Americans have a higher risk for high blood pressure. Poor lifestyle choices and diet, that can be inherited by the family, can also pose as a risk. - A: Arthritis
Some types of arthritis run in families. Genes can be a contributing factor that can make someone susceptible to environmental factors that may trigger arthritis. - L: Lung diseases
Cystic fibrosis is a common inherited disease that affects mostly the lungs. It is manifested by accumulation of thick, sticky mucous, frequent infections and coughing. - D: Diabetes
History of type 2 diabetes in the family poses the patient at increased risk of developing it. - C: Cancers
Certain types of cancer, such as breast cancer and colon cancer, appear more frequently in some families. - H: Heart diseases
Genes can pass on the risk of cardiovascular disease, and they can also be responsible for passing on other conditions such as high blood pressure or high cholesterol levels. - A: Alcoholism
Certain genetic factors influence alcoholism. Research show that children of alcoholics are about four times more likely than the general population to develop alcohol problems. - S: Stroke
Risk for stroke is higher if someone in the patient’s direct family line that stroke. Some strokes may be symptoms of genetic disorders like CADASIL. - M: Mental health disorders (depression, bipolar, schizophrenia etc.)
Some mental illnesses can run in families, although it may be from variety of factors rather than just genes.
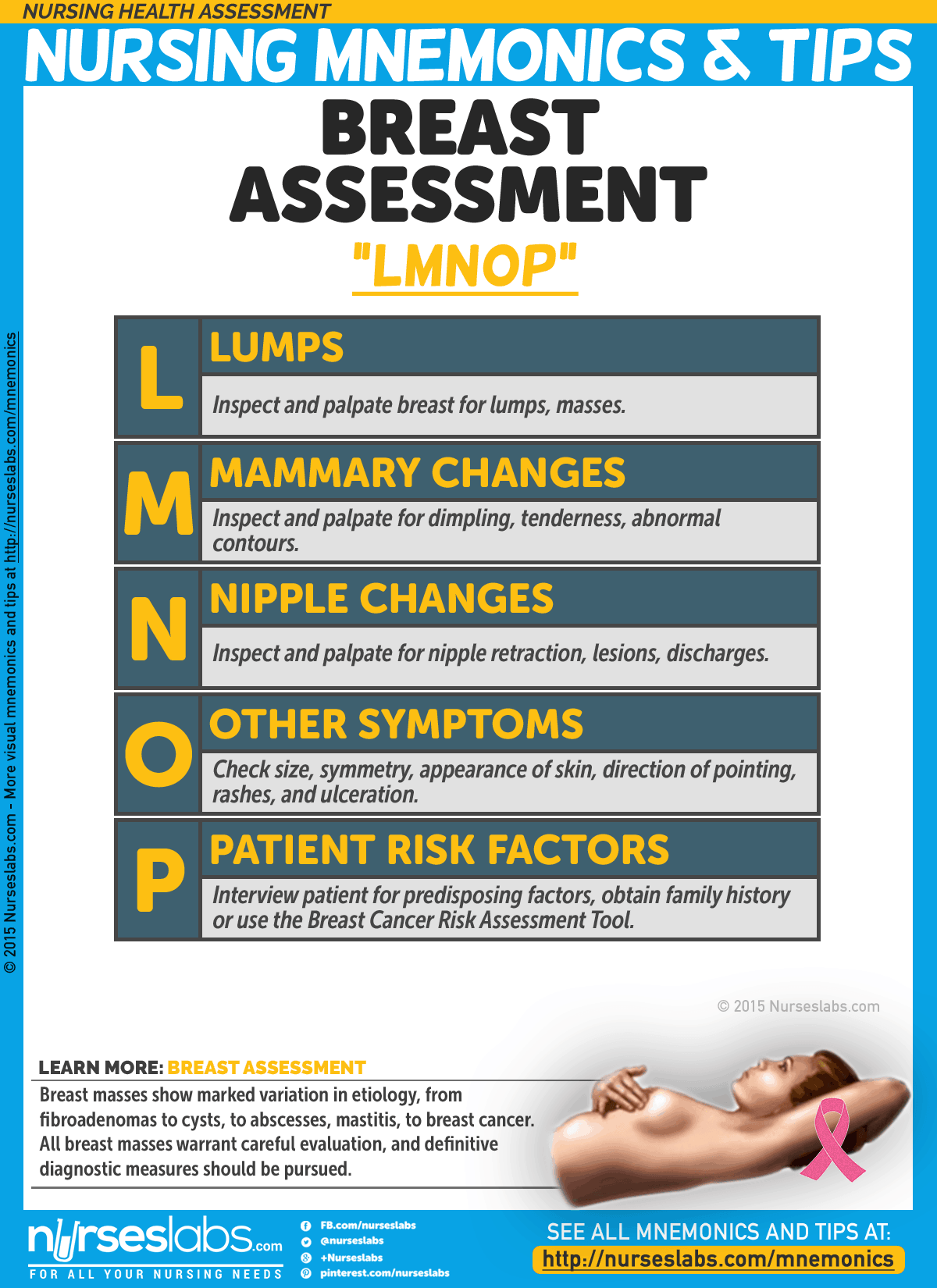
8. Breast Assessment: “LMNOP”
Breast masses show marked variation in etiology, from fibroadenomas to cysts, to abscesses, mastitis, to breast cancer. All breast masses warrant careful evaluation, and definitive diagnostic measures should be pursued.
- L:Lump
Inspect and palpate breast for lumps, masses - M: Mammary changes
Inspect and palpate for dimpling, tenderness, abnormal contours - N: Nipple changes
Inspect and palpate for nipple retraction, lesions, discharges. - O: Other symptoms
Check size, symmetry, appearance of skin, direction of pointing, rashes, and ulceration - P: Patient risk factors
Interview patient for predisposing factors, obtain family history or use the Breast Cancer Risk Assessment Tool.
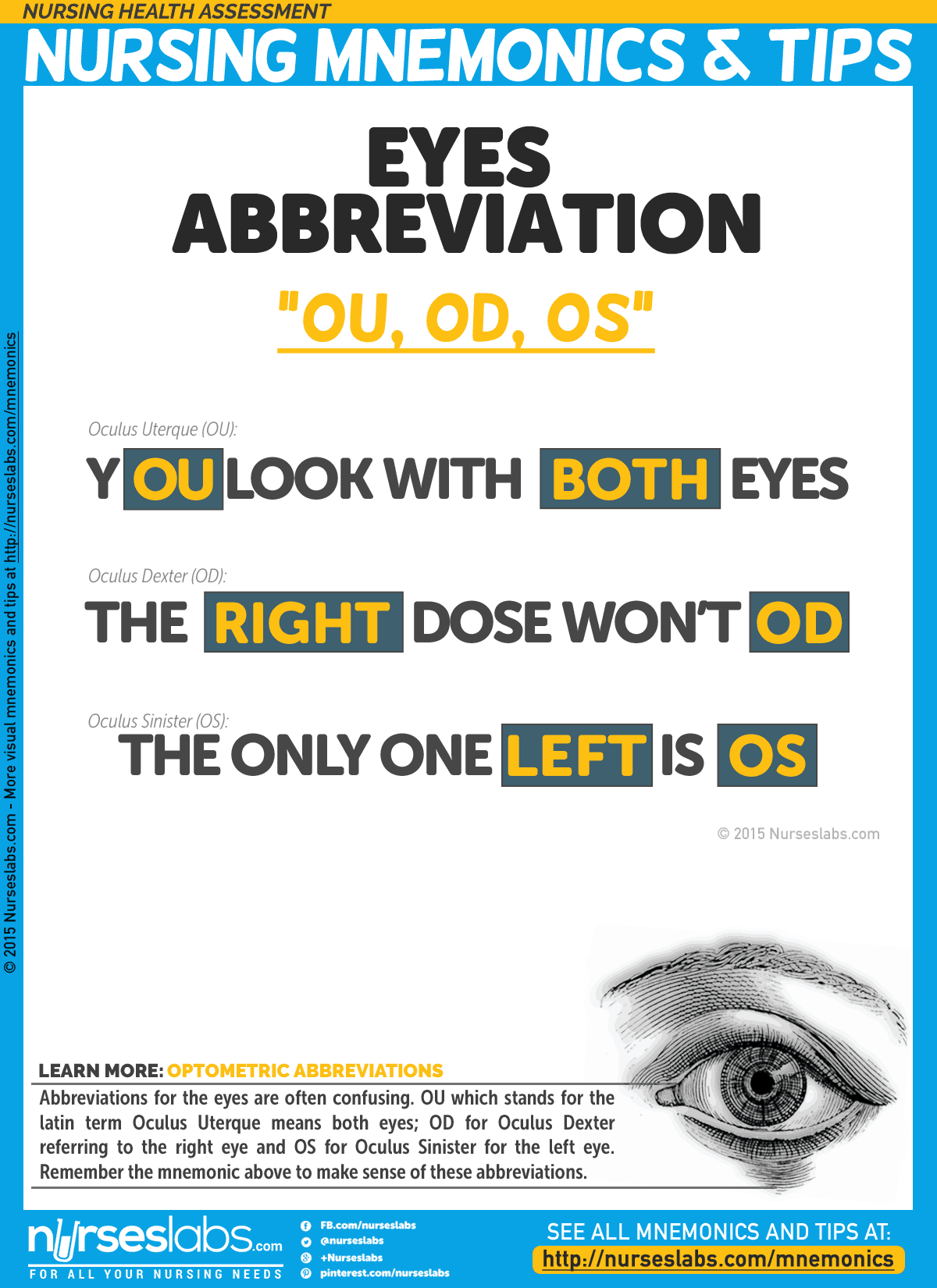
9. Eyes Abbreviation
Abbreviations for the eyes are often confusing. OU which stands for the latin term Oculus Uterque means both eyes; OD for Oculus Dexter referring to the right eye and OS for Oculus Sinister for the left eye. Remember the mnemonic above to make sense of these abbreviations.
- YOU look with BOTH eyes.
- The RIGHT dose won’t OD [overdose].
- The only one that is LEFT is OS.
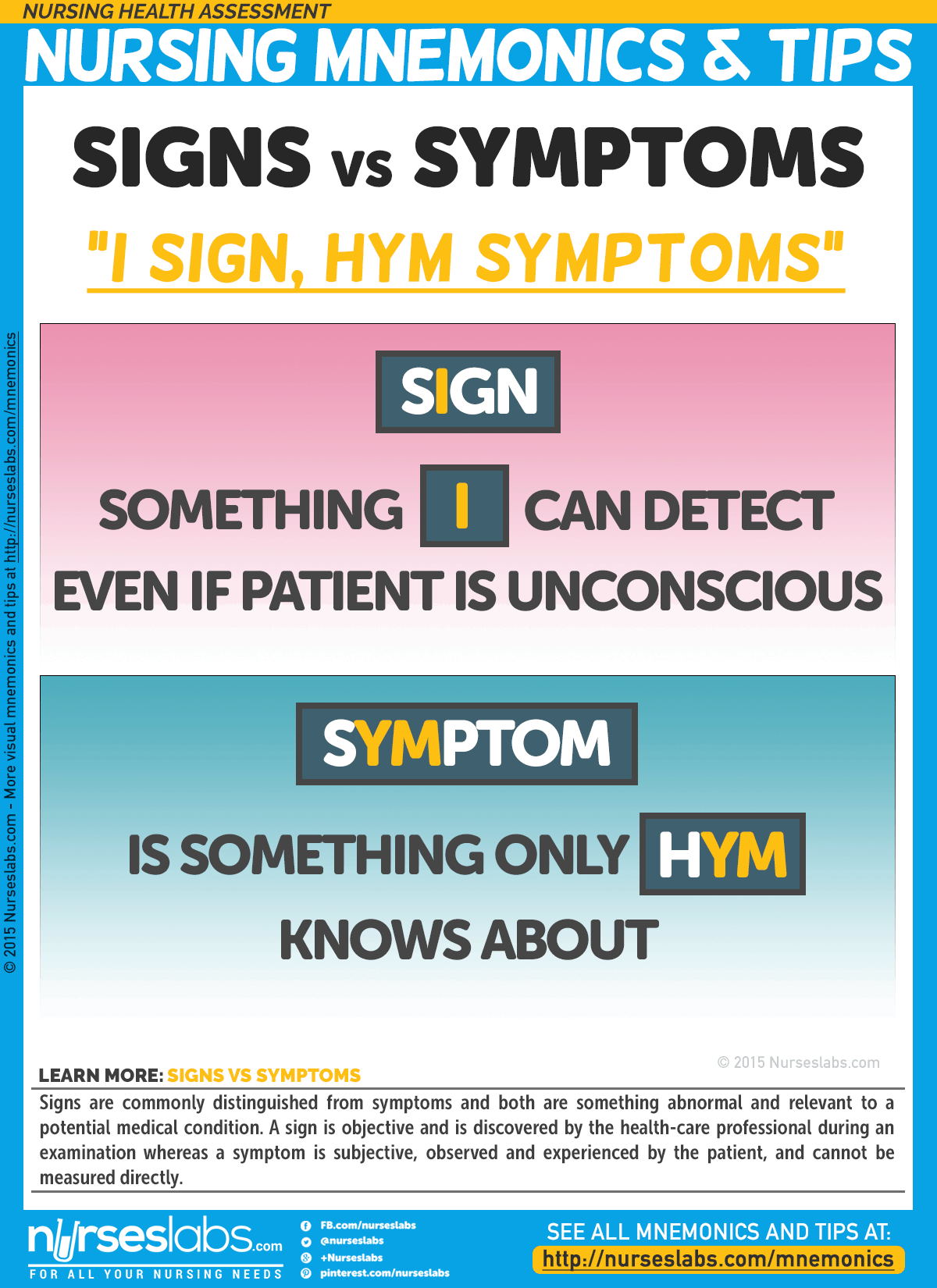
10. Signs VS Symptoms
Signs are commonly distinguished from symptoms and both are something abnormal and relevant to a potential medical condition. A sign is objective and is discovered by the health-care professional during an examination whereas a symptom is subjective, observed and experienced by the patient, and cannot be measured directly.
- sIgn: something I can detect even if patient is unconscious.
- sYMptom is something only hYM knows about.
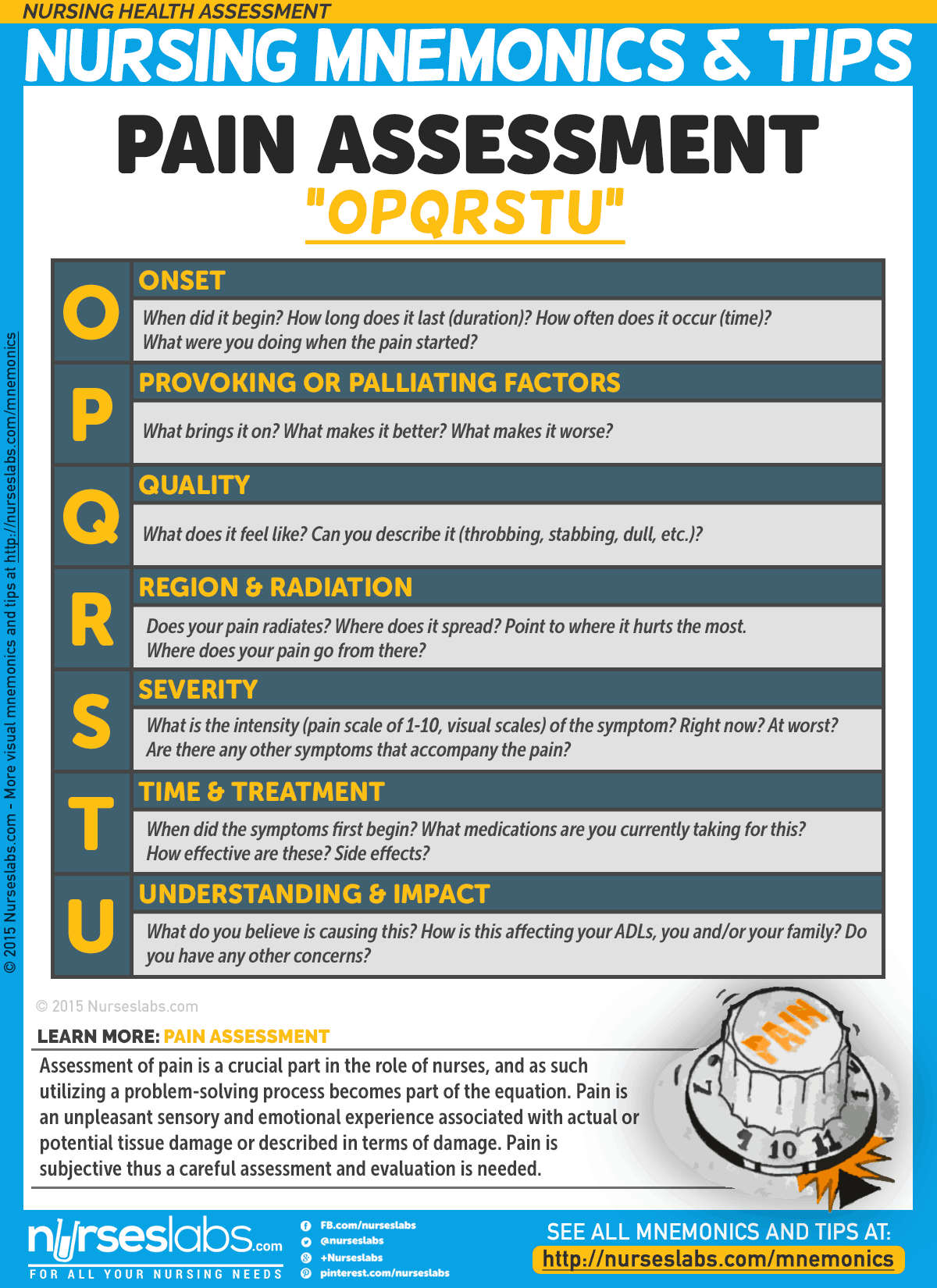
11. Pain Assessment: “OPQRSTU”
Assessment of pain is a crucial part in the role of nurses, and as such utilizing a problem-solving process becomes part of the equation. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of damage. Pain is subjective thus a careful assessment and evaluation is needed.
- O: Onset
When did it begin? How long does it last (duration)? How often does it occur (time)? What were you doing when the pain started? - P: Provoking or Palliating Factors
What brings it on? What makes it better? What makes it worse? - Q: Quality
What does it feel like? Can you describe it (throbbing, stabbing, dull, etc.)? - R: Region & Radiation
Does your pain radiates? Where does it spread? Point to where it hurts the most. Where does your pain go from there? - S: Severity
What is the intensity (pain scale of 1-10, visual scales) of the symptom? Right now? At worst? Are there any other symptoms that accompany the pain? - T: Time & Treatment
When did the symptoms first begin? What medications are you currently taking for this? How effective are these? Side effects? - U: Understanding & Impact
What do you believe is causing this? How is this affecting your ADLs, you and/or your family? - V: Values
What is your goal for this symptom? What is your comfort goal or acceptable level for this symptom? Do you have any other concerns?
More will be added soon…
Know a few witty nursing mnemonics? If you know a few more mnemonics about this topic, please do share them at our comments section below! Else, there are more nursing mnemonics here.






Leave a Comment