Sudden Infant Death Syndrome (SIDS) is a heartbreaking and unexplained phenomenon that claims the lives of seemingly healthy infants during sleep, often leaving families devastated and searching for answers. As nursing professionals, understanding the complexities of SIDS and implementing preventive measures and support for affected families is paramount in reducing its incidence and providing compassionate care to those affected by this tragic loss.
This article aims to serve as a comprehensive nursing guide to SIDS, including its risk factors, prevention strategies, bereavement support, and community education.
What is Sudden Infant Death Syndrome?
Sudden infant death syndrome (SIDS) has caused much grief and anxiety among families for centuries.
- Sudden infant death syndrome (SIDS) are deaths in infants younger than 12 months of age that occur suddenly, unexpectedly, and without obvious cause.
- SIDS cannot be explained despite a thorough investigation, including a complete autopsy, examination of the death scene, and review of the clinical and social history.
- SIDS is also commonly called as “crib death”.
Pathophysiology
Although multiple hypotheses have been proposed as the pathophysiologic mechanisms responsible for SIDS, none have been proven.
- Although both prolongation of the QT interval (long QT syndrome [LQTS]) and shortening of the QT interval (short QT syndrome [SQTS]) are associated with increased risk of cardiac arrhythmia and sudden death, it is QT prolongation that has received the greatest attention in SIDS.
- Clinically, these dysrhythmias may present as syncope, seizures, or sudden cardiac death.
- According to conservative estimates, 30-35% of infants who subsequently die of SIDS have prolongation of the QT interval in the first week of life.
- Other evidence also implicates hypoxia (acute and chronic) in SIDS; hypoxanthine, a marker of tissue hypoxia, is elevated in the vitreous humor of patients who die of SIDS as compared with control subjects who die suddenly.
- Alveolar hypoxia stimulates pulmonary vasoconstriction and, eventually, pulmonary vascular smooth muscle cell hyperplasia.
- Muscularity of the pulmonary vasculature causes pulmonary vasoconstriction, increased right ventricular afterload, and heart failure with more tissue hypoxia.
- Another significant autopsy finding is pleural petechiae, whose formation reflects acute hypoxia in a physiologically intact infant.
Statistics and Incidences
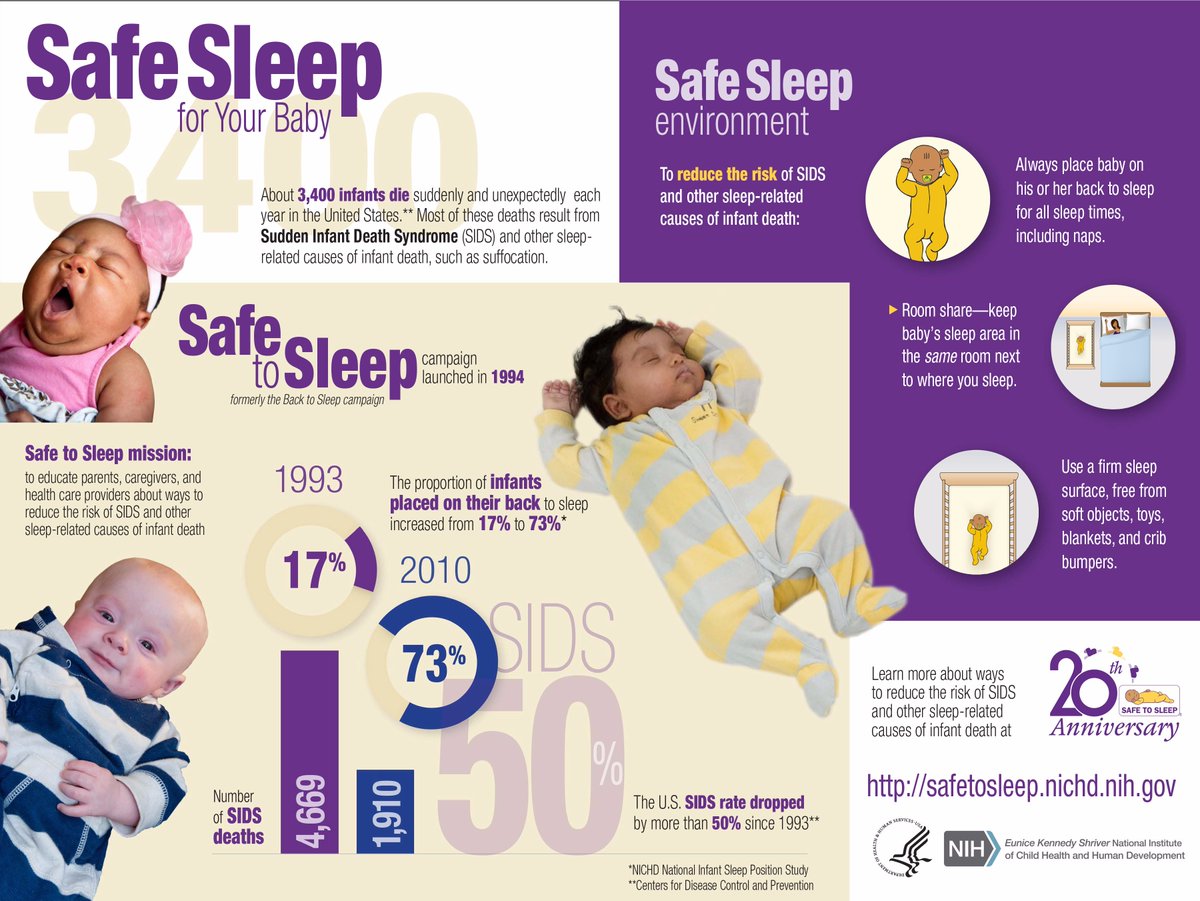
One of the leading causes of infant mortality worldwide, SIDS claims an estimated 2,500 lives annually in the United States alone.
- Although there has been a dramatic drop in the incidence of deaths during the past 20 years, SIDS is still the leading cause of death in infants between 7 and 365 days of age.
- Since 1992, SIDS rates have fallen by approximately 58% in the United States.
- n 1992, the incidence of SIDS was 1.2 cases per 1000 live births; in 2004, the incidence had dropped to 0.51.
- In 2004, 2246 deaths were certified as SIDS, accounting for 8% of infant deaths.
- In 2006, the National Center for Health Statistics reported a total of 2323 SIDS deaths nationwide, for an incidence of 0.54 per 1000 live births.
- In many Asian countries, the current incidence of SIDS is 0.04 per 1000 live births.
- Ninety percent of deaths occur in children younger than 6 months, and 95% of deaths occur in children younger than 8 months; few occur in children younger than 1 month or older than 8 months.
- Approximately 60-70% of SIDS deaths occur in males.
Contributing Factors
Varying theories have been suggested about the cause of SIDS; over the years, much research has been done, but no single cause has been identified. Several authors classify risk factors into groups such as the following:
- Prematurity and low birth weight. Low birth weight, whether resulting from premature birth or from other causes, is associated with a maturational delay in the ability to turn the head to the face-down position.
- Apnea. Regurgitation of gastric contents with acidic pH can cause reflexive apnea with resultant hypoxia.
- Infection. At the time of death, 30-50% of otherwise healthy infants have an acute infection, such as gastroenteritis, otitis media, or, in particular, upper respiratory tract infection (URTI); infantile botulism may be the cause of 5-10% of sudden infant deaths.
- Breastfeeding. A study from New Zealand suggests that infants who are not breastfed are at increased risk for SIDS.
- Maternal smoking. Cigarette smoking during pregnancy is highly significant as a risk factor in the pathogenesis of SIDS.
- Sleeping position and bedtime environment. According to Gilbert-Barness et al, unequivocal evidence indicates that a substantial number (by some estimates, as many as 73.7%) of deaths from SIDS can be prevented by avoiding the prone sleeping position, particularly on any type of soft bedding.
Clinical Manifestations
The classic presentation of sudden infant death syndrome (SIDS) begins with an infant who is put to bed, typically after breastfeeding or bottle-feeding. The observations most commonly reported with Brief Resolved Unexplained Events (BRUEs: formerly Apparent Life-Threatening Events) are as follows:
- Cyanosis. About 50-60% of infants manifests cyanosis.
- Breathing difficulties. Half of the infants who had SIDS experience breathing difficulties before death.
- Abnormal limb movements. Although most of infants are apparently healthy, many parents state that their babies “were not themselves” in the hours before death.
Assessment and Diagnostic Findings
A diagnosis of sudden infant death syndrome (SIDS) is established by excluding recognizable causes of sudden unexplained infant death (SUID).
- Laboratory studies. For a living patient, initial laboratory studies include a complete blood count (CBC), electrolyte concentrations, and urinalysis.
- Radiography and computed tomography scans. Radiographs and computed tomography (CT) scans of the skull may be indicated if abuse is suspected or if signs of increased intracranial pressure are present.
- Histology. In a series of 800 consecutive cases of SUID, [113] 6% of the infants had a neuropathologic cause of death; almost all had clinical histories or gross brain findings at autopsy suggesting the cause of death.
Medical Management
The following measures are done for an infant who experiences SIDS or almost falls victim to it:
- Emergency care. For the infant found in cardiorespiratory arrest, the first priority is life support via attention to the ABCs (Airway, Breathing, Circulation) and other medical interventions as appropriate; in the absence of postmortem lividity or other signs of obvious death, infants must be transported to the hospital to ensure full resuscitative attempts.
- Management of apnea. All infants presenting with nontrivial apnea or apparent life-threatening event (ALTEs) associated with cyanosis or alterations in mental status or tone should be admitted.
- After death. If the infant is pronounced dead, inform the family in a quiet environment. Refer to the child by name, not as “the baby”; detailing resuscitative efforts before telling the parents of the death is not helpful and may engender parents’ resentment; specifically and directly, tell parents that their child has died; use of words such as “dead” or “died” avoids the confusion that may result from gentler terms.
Nursing Management
The effects of SIDS on caregivers and families are devastating.
Nursing Assessment
Assessment of a child before an incidence of SIDS include:
- Physical examination. It is not uncommon for the infant to have been recently examined by a physician and found to be in excellent health.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses for a child with SIDS are:
- Dysfunctional grieving related to sudden, unpredictable death of the infant.
- Interrupted family processes related to grieving.
Nursing Care Planning and Goals
The major nursing care planning goals for the family are:
- Family caregivers will seek appropriate support persons for assistance.
- Family caregivers will use available support systems to assist in coping with fear.
- Family caregivers will share feelings about the event.
- Family caregivers will verbalize measures to prevent SIDS.
Nursing Interventions
Grief is coupled with guilt, even though SIDS cannot be predicted; disbelief, hostility, and anger are common reactions.
- Allow expression of feelings. The immediate reaction of the staff should be to allow the family to express their grief, encouraging them to say goodbye to their infant, and providing a quiet, private place for them to do so.
- Appropriate referrals. Referrals should be made to the local chapter of the National SIDS Foundation immediately; Sudden Infant Death Alliance is another resource for help.
- Encourage use of community resources. In some states, specially trained community health nurses who are knowledgeable about SIDS are available; these nurses are prepared to help families and can provide written materials, as well as information, guidance, and support in the family’s home.
- Monitoring subsequent infants. Caregivers are particularly concerned about subsequent infants; recent studies have indicated that the risk for these infants for the first few months of life to help reduce the family’s stress; monitoring is usually maintained until the new infant is past the age of the SIDS infant’s death.
Evaluation
Goals are met as evidenced by:
- Family caregivers sought appropriate support persons for assistance.
- Family caregivers used available support systems to assist in coping with fear.
- Family caregivers shared feelings about the event.
- Family caregivers verbalized measures to prevent SIDS.
Documentation Guidelines
Documentation in a child with SIDS include:
- Availability and use of support systems and community resources.
- Plan of care.
- Teaching plan.
- Attainment or progress toward desired outcomes.
- Deviations from normal parenting expectations.




























Leave a Comment