Cryptorchidism, also known as undescended testes, is a common congenital anomaly in male infants where one or both testicles fail to descend into the scrotum before birth. Instead, the testes remain within the abdomen or along the inguinal canal. This condition may resolve spontaneously within the first few months of life or require medical intervention to ensure proper testicular descent.
This nursing notes provides an overview of cryptorchidism, discussing its prevalence, clinical manifestations, diagnostic evaluation, treatment options, and the significance of early detection and timely management to promote normal testicular development and reproductive health in affected individuals.
Table of Contents
- What is Cryptorchidism?
- Pathophysiology
- Statistics and Incidences
- Clinical Manifestations
- Assessment and Diagnostic Findings
- Medical Management
- Nursing Management
What is Cryptorchidism?
- Cryptorchidism (from Greek kryptos [“hidden”] and orchis [“testis”]) is the most common abnormality of male sexual development. Shortly before or soon after birth, the male gonads (testes) descend from the abdominal cavity into their normal position in the scrotum.
- Occasionally one or both of the testes do not descend, which is a condition called cryptorchidism.
- Sir John Hunter, the British anatomist, first reported this condition in 1786.
- In 1877, Annandale performed the first successful orchidopexy.
Pathophysiology
Several potential explanations for the pathophysiology of cryptorchidism have been proposed, including gubernacular abnormalities, reduced intra-abdominal pressures, intrinsic testicular or epididymal abnormalities, and endocrine abnormalities, as well as anatomic anomalies.
- The gubernaculum testis is a structure that attaches the lower portion of the tunica vaginalis to the base of the scrotum; the gubernaculum is thought to aid in testicular descent by widening the inguinal canal and guiding the testis down to the scrotum; therefore, anomalies in this attachment may contribute to cryptorchidism.
- Another theory of testicular maldescent is based on intrinsic testicular or epididymal abnormalities; several studies have shown that the germinal epithelium of the maldescended testis may be histologically abnormal.
- Moreover, approximately 23-86% of maldescended testes have been associated with some form of epididymal abnormality; studies have shown an increase in the degree of epididymal abnormalities in intra-abdominal testis in comparison with mild cases of cryptorchidism.
Statistics and Incidences
A palpable undescended testis is found in 3-5% of newborns, and bilateral undescended testis is found in 15% of newborns with cryptorchidism.
- Most undescended palpable testes later spontaneously descend within the first 4 months of life; only 0.7-1% of 1-year-old infants have a persistent undescended testis.
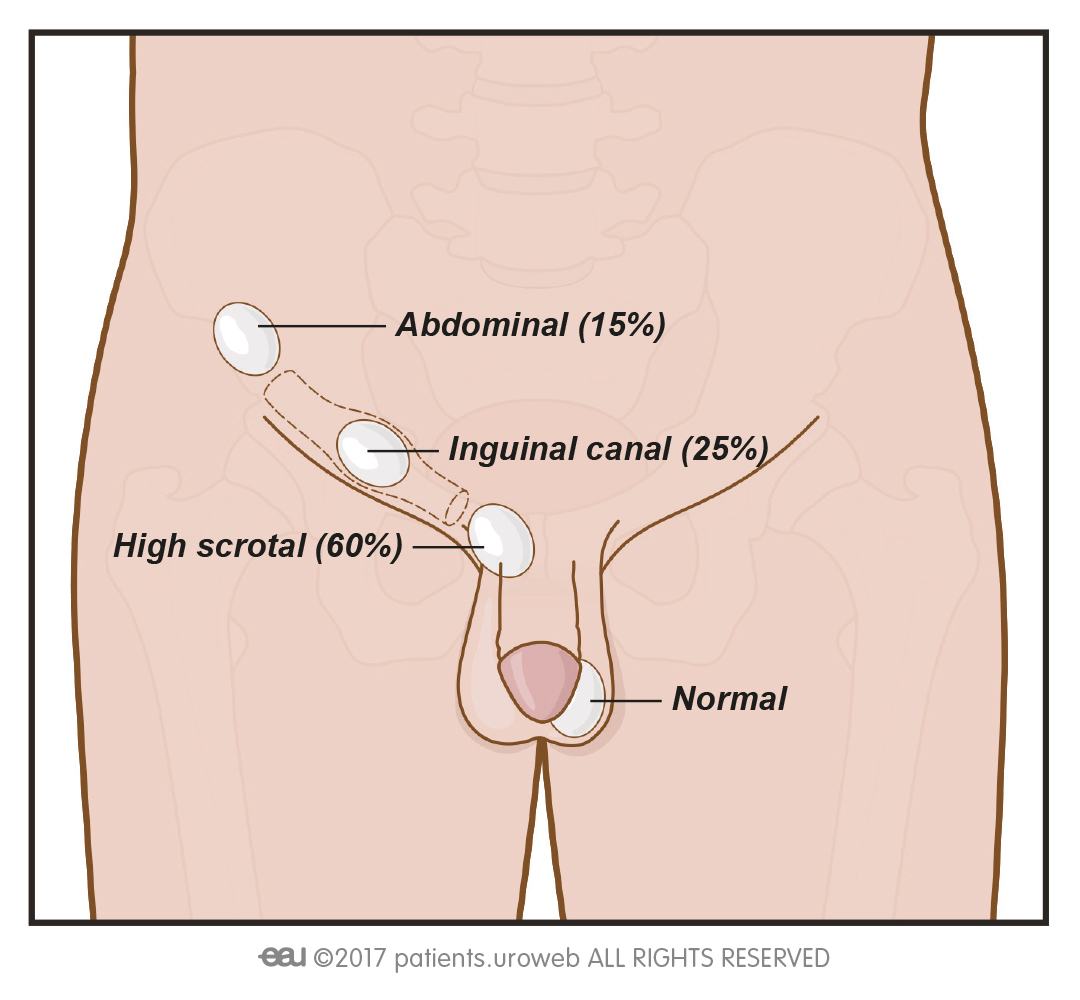
- Nonpalpable testes account for approximately 20% of all undescended testes.
- Approximately 40% of the nonpalpable testes are intra-abdominal, 40% are inguinal, and 20% are atrophic or absent (vanishing testis syndrome).
- Cryptorchidism is found in 30% of babies born prematurely; other predisposing factors include low birth weight, small size for gestational age, twin pregnancy, and maternal estrogen exposure.
- Cryptorchidism is found in 7% of siblings and in about 2% of fathers of babies with this condition.
- Cryptorchidism affects only males and has no reported racial predilection.
Clinical Manifestations
Determining if the testis was palpable in the scrotum at any time is important.
- Hemiscrotal asymmetry. Upon observation, the scrotum is not symmetrical.
- Contralateral testicular hypertrophy. This is an indicator of an absent testis.
Assessment and Diagnostic Findings
Laboratory tests and imaging studies are unnecessary in diagnosing cryptorchidism.
- Diagnostic laparoscopy. Diagnostic laparoscopy is the most reliable technique for localizing the nonpalpable testis; it is performed in conjunction with definitive therapy (laparoscopic orchiopexy or open orchiopexy).
- Histologic findings. The histologic findings of an undescended testis range from normal histology to acquired germ-cell hypoplasia with Leydig cell hyperplasia; the severity of the histologic findings is correlated with an intra-abdominal testis, delayed orchiopexy, or both.
Medical Management
Engle proposed hormonal manipulation as a treatment for cryptorchidism in the 1930s. The main goals of treatment, whether hormonal or surgical, are as follows: to allow the testicle to occupy a normal anatomic position; to preserve fertility and hormonal production
; and to diagnose potential testicular malignancies.
- Hormonal therapy. Hormonal therapy should be considered for patients in whom the diagnosis of retractile testis is not certain; hormonal therapy has been employed in Europe for many years as a primary therapy for cryptorchidism; the main hormones used are human chorionic gonadotropin (hCG) and luteinizing hormone (LH)-releasing hormone (LHRH); in Europe, these two hormones have been given in combination, with initial success rates of 14-65%; however, some long-term studies have shown lower success rates.
- Orchiopexy. A surgical procedure called orchiopexy is used to bring the testis down into the scrotum and anchor it there; surgery is usually performed when the child is 1 to 2 years old; prognosis for a normal functioning testicle is good when the surgery is performed at this young age and no degenerative action has taken place before treatment.
Nursing Management
Nursing care of a child with cryptorchidism includes the following:
Nursing Assessment
Assessment of the child involves:
- History. Obtain history from prenatal and birth records, and through interviews with family caregivers.
- Physical examination. Physical examination is the most important tool in the diagnostic evaluation of cryptorchidism; the patient must be examined in a warm, relaxed environment; closely observing the scrotum before manipulation is important; the frog-leg or catcher position may be used to facilitate palpation of the testis.
Nursing Diagnoses
Based on the assessment data, the major nursing diagnoses are:
- Impaired urinary elimination related to the condition and surgical intervention.
- Disturbed body image related to the appearance of the genitalia.
- Risk for infection related to surgical incision and drainage tubes.
- Deficient knowledge related to the condition and surgery.
Nursing Care Planning and Goals
The major goals for the patient are:
- The patient will have clear urine draining from the catheter.
- The family caregivers will be able to verbalize an understanding of the condition and the surgical intervention.
- The patient will be free from infection.
- The patient will have relief from pain and discomfort.
- The patient will exhibit adequate urine output.
Nursing Interventions
The nursing interventions appropriate for the patient are:
- Understanding the surgical treatment. Determine the child’s expectations regarding illness and hospitalization through discussion and play therapy; explain the anatomy and physiology of the urinary system in terms the child can understand; use a body outline appropriate for the age of the child, and explain all diagnostic tests before their occurrence.
- Promoting normal urine output. Monitor daily intake and output; encourage adequate fluids and monitor daily weights; care for all catheters and urinary tubes according to facility policy; maintain the appropriate position of tubes; observe and record amount and appearance of urinary drainage, the occurrence of bladder spasms, and symptoms of urinary or incisional infection.
- Providing emotional support regarding body image. Continue reassurance about the appearance of genitalia; maintain discussions regarding reactions; this may need to be done with patient and family alone as well as a family unit; discuss plans for interim period from initial surgery until secondary or reconstructive procedures can be performed; initiate independence of care; and focus on activities the child can perform and accomplish.
- Preventing infection. Administer antibiotics and I.V. fluids as ordered; maintain patency of catheters; provide catheter care as directed; administer wound care using aseptic technique, and inspect incision for drainage or signs of infection.
- Maintaining fluid volume. Administer fluids as ordered; monitor vital signs for hypotension or tachycardia; assess patient’s skin turgor and mucous membranes for signs of dehydration; measure and record accurate intake and output.
- Promoting comfort. Administer analgesics as ordered and according to the assessment of complaints of pain, restlessness, crying, or withdrawal; administer antispasmodics as ordered for bladder spasms, and provide distraction and comfort measures.
Evaluation
Goals are met as evidenced by:
- The patient has clear urine draining from the catheter.
- The family caregivers verbalized understanding of the condition and the surgical intervention.
- The patient is free from infection.
- The patient has relief from pain and discomfort.
- The patient exhibited adequate urine output.
Documentation Guidelines
Documentation in a patient with cryptorchidism includes:
- Individual findings include factors affecting, interactions, the nature of social exchanges, and specifics of individual behavior.
- Intake and output.
- Signs of infection.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.