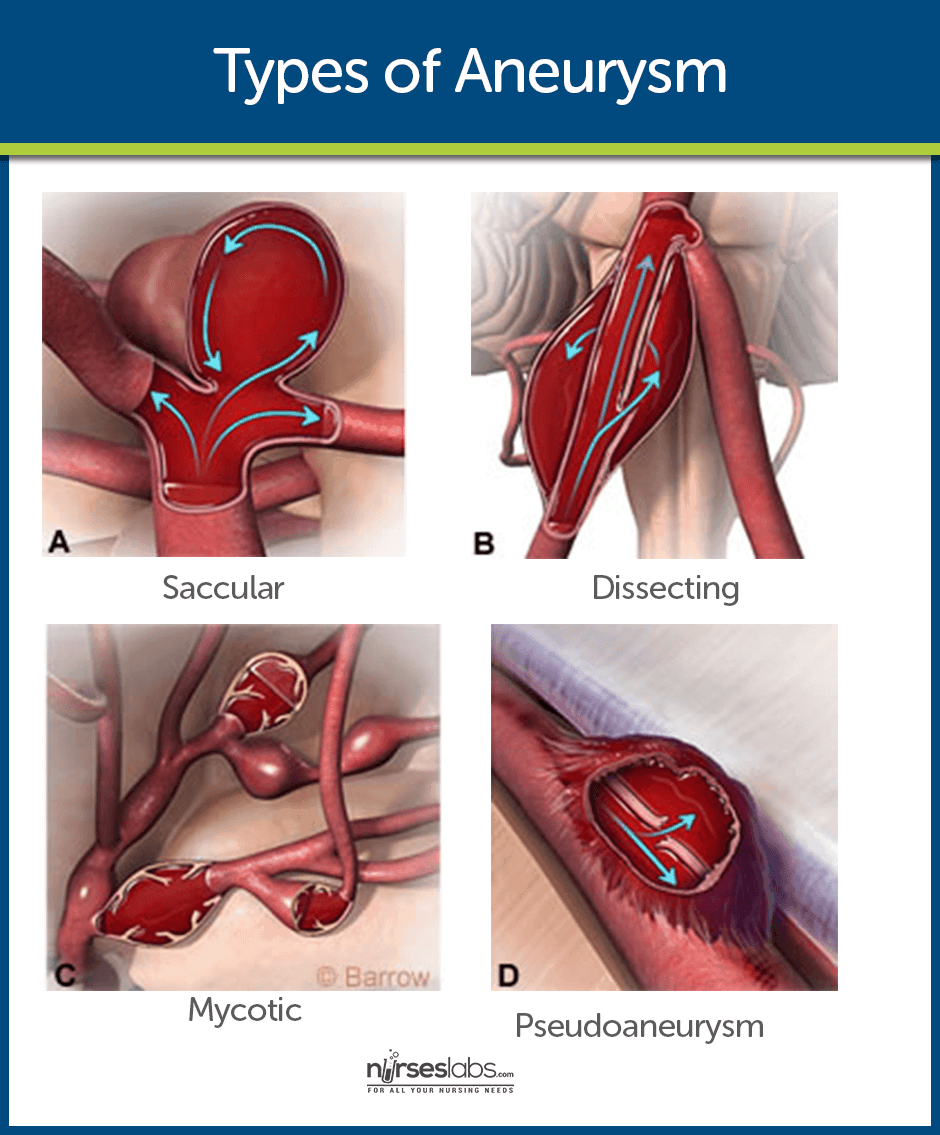
An intracranial aneurysm is a dilation of the walls of a cerebral artery that develops as a result of weakness in the arterial wall.
What is Intracranial Aneurysm?
Hemorrhagic strokes are caused by bleeding into the brain tissue, the ventricles, or the subarachnoid space, and the intracranial aneurysm is one of them.
- An intracranial aneurysm is a dilation of the walls of a cerebral artery that develops as a result of weakness in the arterial wall.
- Subarachnoid hemorrhage results from a ruptured intracranial aneurysm.
Pathophysiology
The pathophysiology of intracranial aneurysms depends on the cause and type of cerebrovascular disorder.
- Disruption. Normal brain metabolism is disrupted by the brain’s exposure to blood.
- Increase in ICP. An increase in ICP starts from the sudden entry of blood into the subarachnoid space.
- Injury. Compression and injury occur in the brain tissue.
Statistics and Incidences
Intracranial aneurysm accounts for half of the cases of hemorrhagic strokes.
- The mortality rate has been reported as high as 48% at 30 days after an intracranial hemorrhage.
- Hemorrhagic strokes account for 15% to 20% of cerebrovascular disorders and ate primarily caused by intracranial hemorrhage.
- Primary intracerebral hemorrhage from a spontaneous rupture of small vessels accounts for approximately 80% of hemorrhagic strokes.
Causes
The cause of the aneurysm is unknown, although research is ongoing.
- Atherosclerosis. Fatty plaques lining the blood vessels in the brain could lead to aneurysm.
- Congenital defect of the vessel wall. The defect has been there at the moment of birth and could cause serious intracranial aneurysm.
- Hypertensive vascular disease. Uncontrolled hypertension could rupture the small vessels in the brain and lead to an intracranial aneurysm.
Clinical Manifestations
Symptoms are produced when an aneurysm presses on nearby cranial nerves or brain tissue.
- Severe headache. The conscious patient most commonly reports a severe headache.
- Increased ICP. An increased ICP could cause vomiting.
- Sudden change in the level of consciousness. As the aneurysm presses on nerves and tissues, there is a sudden early change in the level of consciousness.
- Focal seizures. Focal seizures can possibly occur due to frequent brain stem involvement.
- Nuchal rigidity. There may be pain and rigidity of the back of the neck and spine due to irritation.
- Visual disturbances. Visual loss, diplopia, and ptosis occur if the aneurysm is adjacent to the oculomotor nerve.
Prevention
Primary prevention is the best approach.
- Hypertension. Control of hypertension, especially in people older than 55 years old, reduces the risk.
- Stroke risk screenings. Stroke risk screenings provide an ideal opportunity to lower the risk by identifying high-risk individuals or groups.
- Education. Educating patients and the community about recognition and prevention can reduce the risk.
Complications
Possible complications of hemorrhagic stroke include:
- Bleeding. Hematoma expansion is a fatal complication.
- Cerebral vasospasm. Cerebral vasospasm resulting in cerebral ischemia is also one of the risk factors.
- Acute hydrocephalus. Acute hydrocephalus results when free blood obstructs the reabsorption of cerebrospinal fluid by the arachnoid villi.
- Focal seizures. Seizures may occur because of extreme nerve irritation.
Assessment and Diagnostic Findings
Any patient with a suspected stroke should undergo the following:
- CT scan or MRI. These studies determine the type of stroke, the size and location of the hematoma, and the presence or absence of ventricular blood and hydrocephalus.
- Cerebral angiography. Cerebral angiography confirms the diagnosis of an intracranial aneurysm.
- Lumbar puncture. Lumbar puncture is performed if there is no evidence of increased ICP, the CT scan results are negative, and subarachnoid hemorrhage must be confirmed.
Medical Management
The goals of medical treatment are to allow the brain to recover from the initial insult, to prevent or minimize the risk of rebleeding, and to prevent or treat complications.
- Bed rest. Bed rest with sedation can prevent agitation and stress.
- Fresh frozen plasma and vitamin K. If the bleeding is caused by anticoagulation with warfarin, the INR may be corrected with FFP and vitamin K.
- Antiseizure agents. Because seizures can occur after intracerebral hemorrhage, antiseizure agents are often administered prophylactically for a brief period of time.
- Analgesic agents. Analgesic agents may be prescribed for head and neck pain.
- Sequential compression devices. Sequential compression devices or anti-embolism stockings prevent deep vein thrombosis.
Surgical Management
The goal of surgery is to prevent bleeding in an unruptured aneurysm or further bleeding in an already ruptured aneurysm.
- Craniotomy. Surgical evacuation is most frequently accomplished via a craniotomy.
- Endovascular treatment. This is the surgical management for the occlusion of the parent artery.
- Aneurysm coiling. This is the obstruction of the aneurysm site with a coil.
Nursing Management
All patients should be monitored in the intensive care unit after an intracerebral aneurysm.
Nursing Assessment
A complete neurologic assessment is performed initially and includes evaluation for the following:
- Altered level of consciousness.
- Sluggish pupillary reaction.
- Motor and sensory dysfunction.
- Cranial nerve deficits (extraocular eye movements, facial droop, presence of ptosis).
- Speech difficulties and visual disturbance.
- Headache and nuchal rigidity or other neurologic deficits.
Nursing Diagnosis
Based on the assessment data, the patient’s major nursing diagnoses may include the following:
- Ineffective tissue perfusion related to bleeding or vasospasm.
- Disturbed sensory perception related to medically imposed restrictions.
- Anxiety related to illness and/or medically imposed restrictions (aneurysm precautions).
Nursing Care Planning & Goals
Main Article: 8 Cerebrovascular Accident (Stroke) Nursing Care Plans
The goals for the patient may include:
- Improve cerebral tissue perfusion.
- Relief of sensory and perceptual deprivation.
- Relief of anxiety.
- Absence of complications.
Nursing Interventions
All patients should be monitored in the intensive care unit after an intracerebral hemorrhage.
Improving Cerebral Tissue Perfusion
- Monitor closely for neurologic deterioration, and maintain a neurologic flow record.
- Check blood pressure, pulse, level of consciousness, pupillary responses, and motor function hourly; monitor respiratory status and report changes immediately.
- Implement aneurysm precautions (immediate and absolute bed rest in a quiet, nonstressful setting; restrict visitors, except for family).
- Elevate the head of the bed 15 to 30 degrees or as ordered.
- Avoid any activity that suddenly increases blood pressure or obstructs venous return (eg, Valsalva maneuver, straining), instructs the patient to exhale during voiding or defecation to decrease strain, eliminate caffeine, administer all personal care, and minimize external stimuli.
- Apply anti-embolism stockings or sequential compression devices. Observe legs for signs and symptoms of deep vein thrombosis tenderness, redness, swelling, warmth, and edema.
Relieving Sensory Deprivation
- Keep sensory stimulation to a minimum.
- Explain restrictions to help reduce the patient’s sense of isolation.
- Relieving Anxiety
- Inform patient of plan of care.
- Provide support and appropriate reassurance to patient and family.
Monitoring and Managing Potential Complications
- Assess for and immediately report signs of possible vasospasm, which may occur several days after surgery or on the initiation of treatment (intensified headaches, decreased level of responsiveness, or evidence of aphasia or partial paralysis). Also, administer calcium channel blockers or fluid volume expanders as prescribed.
- Maintain seizure precautions. Also, maintain airway and prevent injury if a seizure occurs. Administer antiseizure medications as prescribed (phenytoin [Dilantin] is the medication of choice).
- Monitor for the onset of symptoms of hydrocephalus, which may be acute (first 24 hours after hemorrhage), subacute (days later), or delayed (several weeks later). Report symptoms immediately: acute hydrocephalus is characterized by sudden stupor or coma; subacute or delayed is characterized by gradual onset of drowsiness, behavioral changes, and ataxic gait.
- Monitor for and report symptoms of aneurysm rebleeding. Rebleeding occurs most often in the first 2 weeks.
- Symptoms include sudden severe headache, nausea, vomiting, decreased level of consciousness, and neurologic deficit.
- Administer medications as ordered.
- Hyponatremia: monitor laboratory data often because hyponatremia (serum sodium level under 135 mEq/L) affects up to 30% of patients. Report low levels persisting for 24 hours, as a syndrome of inappropriate antidiuretic hormone (SIADH) or cerebral salt wasting syndrome (kidneys cannot conserve sodium) may develop.
Teaching Patients Self Care
- Provide the patient and family with information to promote cooperation with the care and required activity restrictions and prepare them for the patient’s return home.
- Identify the causes of intracranial hemorrhage, its possible consequences, and the medical or surgical treatments that are implemented. Discuss the importance of interventions taken to prevent and detect complications (eg, aneurysm precautions, close monitoring of patient). As indicated, facilitate transfer to a rehabilitation unit or center.
Evaluation
Expected patient outcomes may include the following:
- Improved cerebral tissue perfusion.
- Relief of sensory and perceptual deprivation.
- Relief of anxiety.
- Absence of complications.
Discharge and Home Care Guidelines
The patient and the family are provided with information that will enable them to cooperate with the care and restrictions required to prepare them to return home.
- Causes. Patient and family teaching includes information about the causes of intracranial aneurysm and its possible consequences.
- Medical treatments. The patient and the family are informed about the medical treatments that are implemented, including the surgical intervention and the importance of interventions taken to prevent and improve cerebral tissue perfusion.
- Assistive devices and environment. Teaching addresses the use of assistive devices or modification of the home environment to help the patient live with the disability.
- Follow-up appointments. The patient and family are reminded of the importance of following recommendations and keeping with follow-up appointments with healthcare providers for monitoring of risk factors.
Documentation Guidelines
The focus of documentation in a patient with an intracranial aneurysm includes:
- Extent, nature, and duration of the problem.
- Effects on independence and lifestyle.
- Pulses and BP.
- Assistive device needs.
- Plan of care.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
- Modifications to plan of care.
- Long-term needs.
See Also
Posts related to this care plan:
























Leave a Comment