Writing the best nursing care plan requires a step-by-step approach to complete the parts needed for a care plan correctly. This tutorial will walk you through developing a care plan. This guide has the ultimate database and list of nursing care plans (NCP) and nursing diagnosis samples for our student nurses and professional nurses to use—all for free! Care plan components, examples, objectives, and purposes are included with a detailed guide on writing an excellent nursing care plan or a template for your unit.
What is a Nursing Care Plan?
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes a client’s potential needs or risks. Care plans provide a way of communication among nurses, their patients, and other healthcare providers to achieve healthcare outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
Nursing care planning begins when the client is admitted to the agency and is continuously updated throughout in response to the client’s changes in condition and evaluation of goal achievement. Planning and delivering individualized or patient-centered care is the basis for excellence in nursing practice.
Types of Nursing Care Plans
Care plans can be informal or formal: An informal nursing care plan is a strategy of action that exists in the nurse’s mind. A formal nursing care plan is a written or computerized guide that organizes the client’s care information.
Formal care plans are further subdivided into standardized care plans and individualized care plans: Standardized care plans specify the nursing care for groups of clients with everyday needs. Individualized care plans are tailored to meet a specific client’s unique needs or needs that are not addressed by the standardized care plan.
Standardized Care Plans
Standardized care plans are pre-developed guides by the nursing staff and health care agencies to ensure that patients with a particular condition receive consistent care. These care plans are used to ensure that minimally acceptable criteria are met and to promote the efficient use of the nurse’s time by removing the need to develop common activities that are done repeatedly for many of the clients on a nursing unit.
Standardized care plans are not tailored to a patient’s specific needs and goals and can provide a starting point for developing an individualized care plan.
Care plans listed in this guide are standard care plans which can serve as a framework or direction to develop an individualized care plan.
Individualized Care Plans
An individualized care plan care plan involves tailoring a standardized care plan to meet the specific needs and goals of the individual client and use approaches shown to be effective for a particular client. This approach allows more personalized and holistic care better suited to the client’s unique needs, strengths, and goals.
Additionally, individualized care plans can improve patient satisfaction. When patients feel that their care is tailored to their specific needs, they are more likely to feel heard and valued, leading to increased satisfaction with their care. This is particularly important in today’s healthcare environment, where patient satisfaction is increasingly used as a quality measure.
Tips on how to individualize a nursing care plan:
- Perform a comprehensive assessment of the patient’s health, history, health status, and desired goals.
- Involve the patient in the care planning process by asking them about their health goals and preferences. By involving the client, nurses can ensure that the care plan is aligned with the patient’s goals and preferences which can improve patient engagement and compliance with the care plan.
- Perform an ongoing assessment and evaluation as the patient’s health and goals can change. Adjust the care plan accordingly.
Objectives
The following are the goals and objectives of writing a nursing care plan:
- Promote evidence-based nursing care and render pleasant and familiar conditions in hospitals or health centers.
- Support holistic care, which involves the whole person, including physical, psychological, social, and spiritual, with the management and prevention of the disease.
- Establish programs such as care pathways and care bundles. Care pathways involve a team effort to reach a consensus regarding standards of care and expected outcomes. In contrast, care bundles are related to best practices concerning care for a specific disease.
- Identify and distinguish goals and expected outcomes.
- Review communication and documentation of the care plan.
- Measure nursing care.
Purposes of a Nursing Care Plan
The following are the purposes and importance of writing a nursing care plan:
- Defines nurse’s role. Care plans help identify nurses’ unique and independent role in attending to clients’ overall health and well-being without relying entirely on a physician’s orders or interventions.
- Provides direction for individualized care of the client. It serves as a roadmap for the care that will be provided to the patient and allows the nurse to think critically in developing interventions directly tailored to the individual.
- Continuity of care. Nurses from different shifts or departments can use the data to render the same quality and type of interventions to care for clients, therefore allowing clients to receive the most benefit from treatment.
- Coordinate care. Ensures that all members of the healthcare team are aware of the patient’s care needs and the actions that need to be taken to meet those needs preventing gaps in care.
- Documentation. It should accurately outline which observations to make, what nursing actions to carry out, and what instructions the client or family members require. If nursing care is not documented correctly in the care plan, there is no evidence the care was provided.
- Serves as a guide for assigning a specific staff to a specific client. There are instances when a client’s care needs to be assigned to staff with particular and precise skills.
- Monitor progress. To help track the patient’s progress and make necessary adjustments to the care plan as the patient’s health status and goals change.
- Serves as a guide for reimbursement. The insurance companies use the medical record to determine what they will pay concerning the hospital care received by the client.
- Defines client’s goals. It benefits nurses and clients by involving them in their treatment and care.
Components
A nursing care plan (NCP) usually includes nursing diagnoses, client problems, expected outcomes, nursing interventions, and rationales. These components are elaborated on below:
- Client health assessment, medical results, and diagnostic reports are the first steps to developing a care plan. In particular, client assessment relates to the following areas and abilities: physical, emotional, sexual, psychosocial, cultural, spiritual/transpersonal, cognitive, functional, age-related, economic, and environmental. Information in this area can be subjective and objective.
- Nursing diagnosis. A nursing diagnosis is a statement that describes the patient’s health issue or concern. It is based on the information gathered about the patient’s health status during the assessment.
- Expected client outcomes. These are specific goals that will be achieved through nursing interventions. These may be long and short-term.
- Nursing interventions. These are specific actions that will be taken to address the nursing diagnosis and achieve expected outcomes. They should be based on best practices and evidence-based guidelines.
- Rationales. These are evidence-based explanations for the nursing interventions specified.
- Evaluation. These includes plans for monitoring and evaluating a patient’s progress and making necessary adjustments to the care plan as the patient’s health status and goals change.
Care Plan Formats
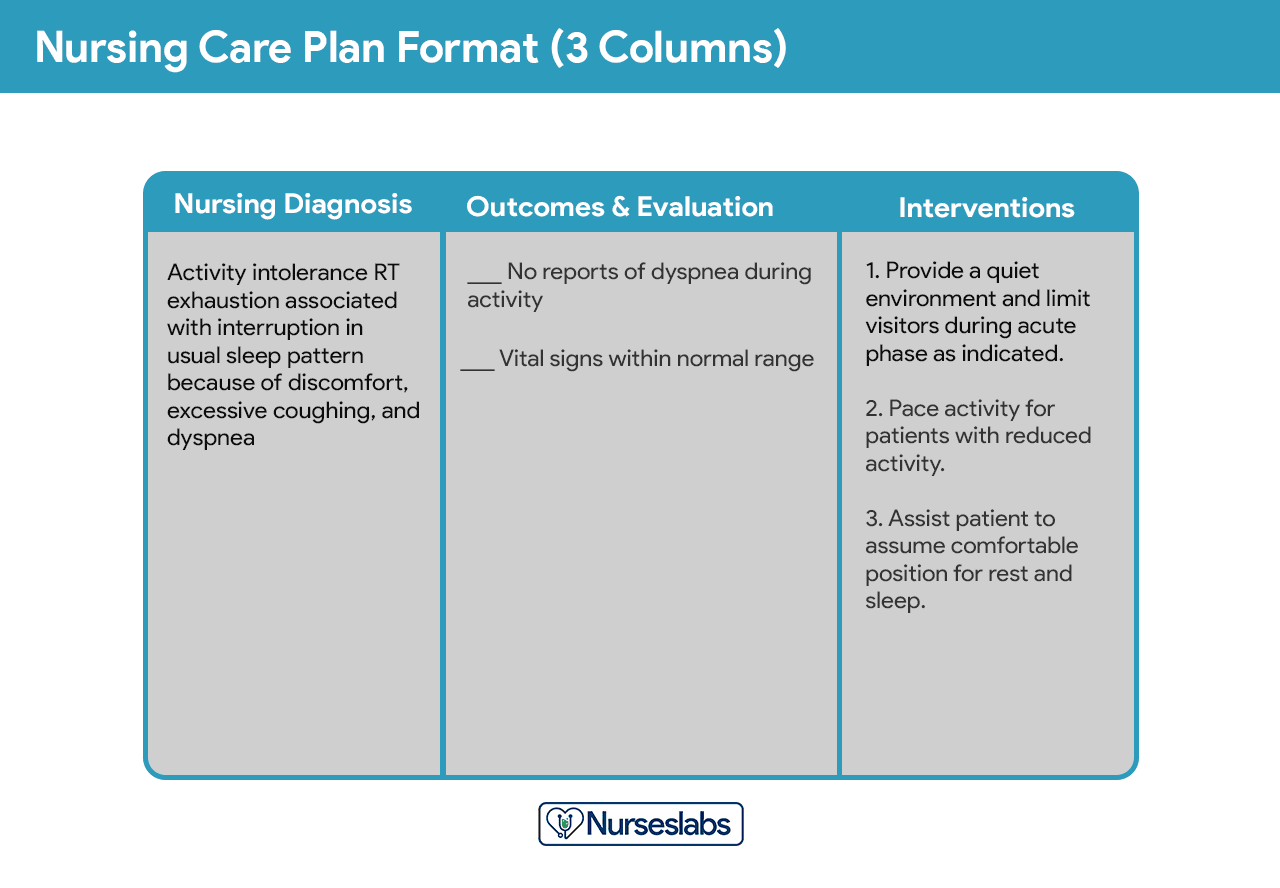
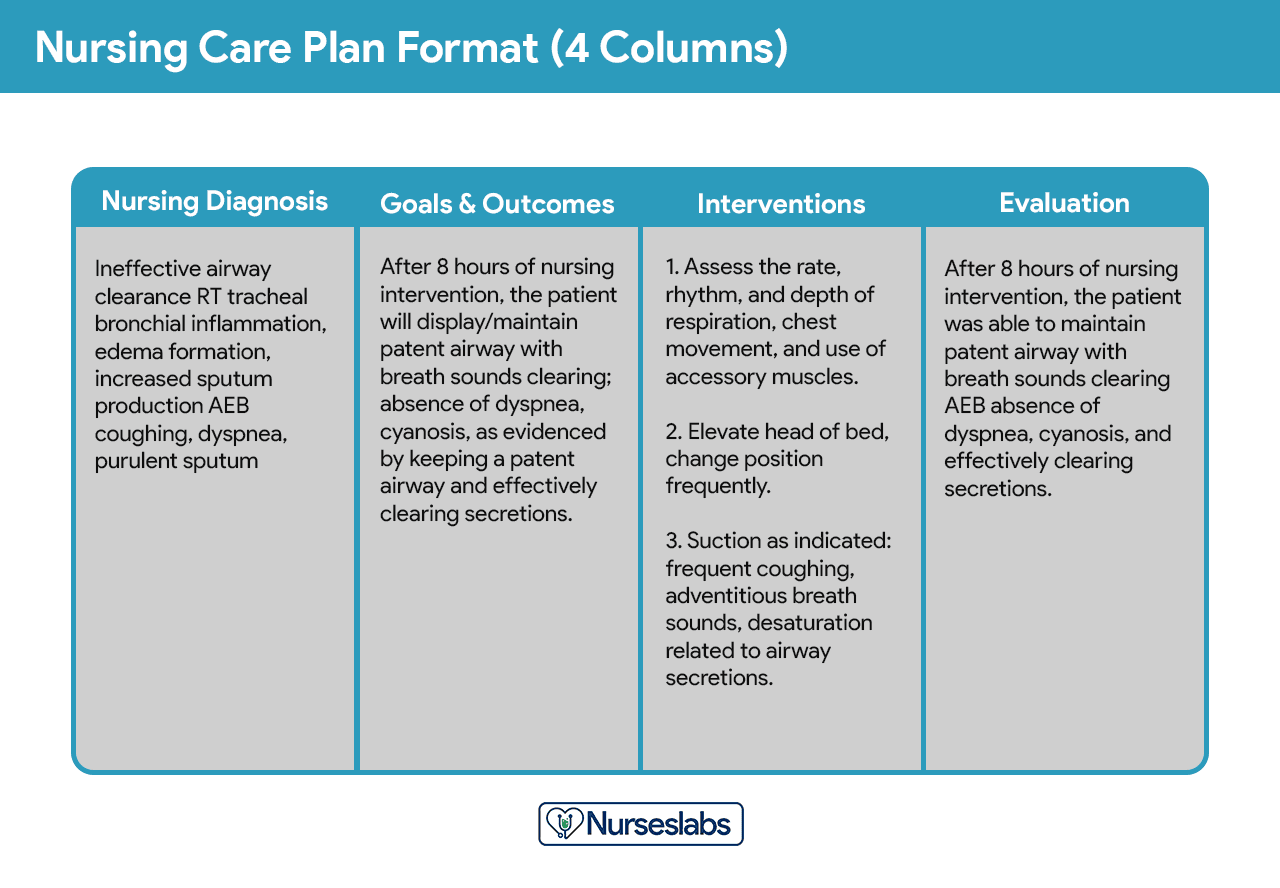
Nursing care plan formats are usually categorized or organized into four columns: (1) nursing diagnoses, (2) desired outcomes and goals, (3) nursing interventions, and (4) evaluation. Some agencies use a three-column plan where goals and evaluation are in the same column. Other agencies have a five-column plan that includes a column for assessment cues.
Three-Column Format
The three-column plan has a column for nursing diagnosis, outcomes and evaluation, and interventions.
Four-Column Format
This format includes columns for nursing diagnosis, goals and outcomes, interventions, and evaluation.
Below is a document containing sample templates for the different nursing care plan formats. Please feel free to edit, modify, and share the template.
Download: Printable Nursing Care Plan Templates and Formats
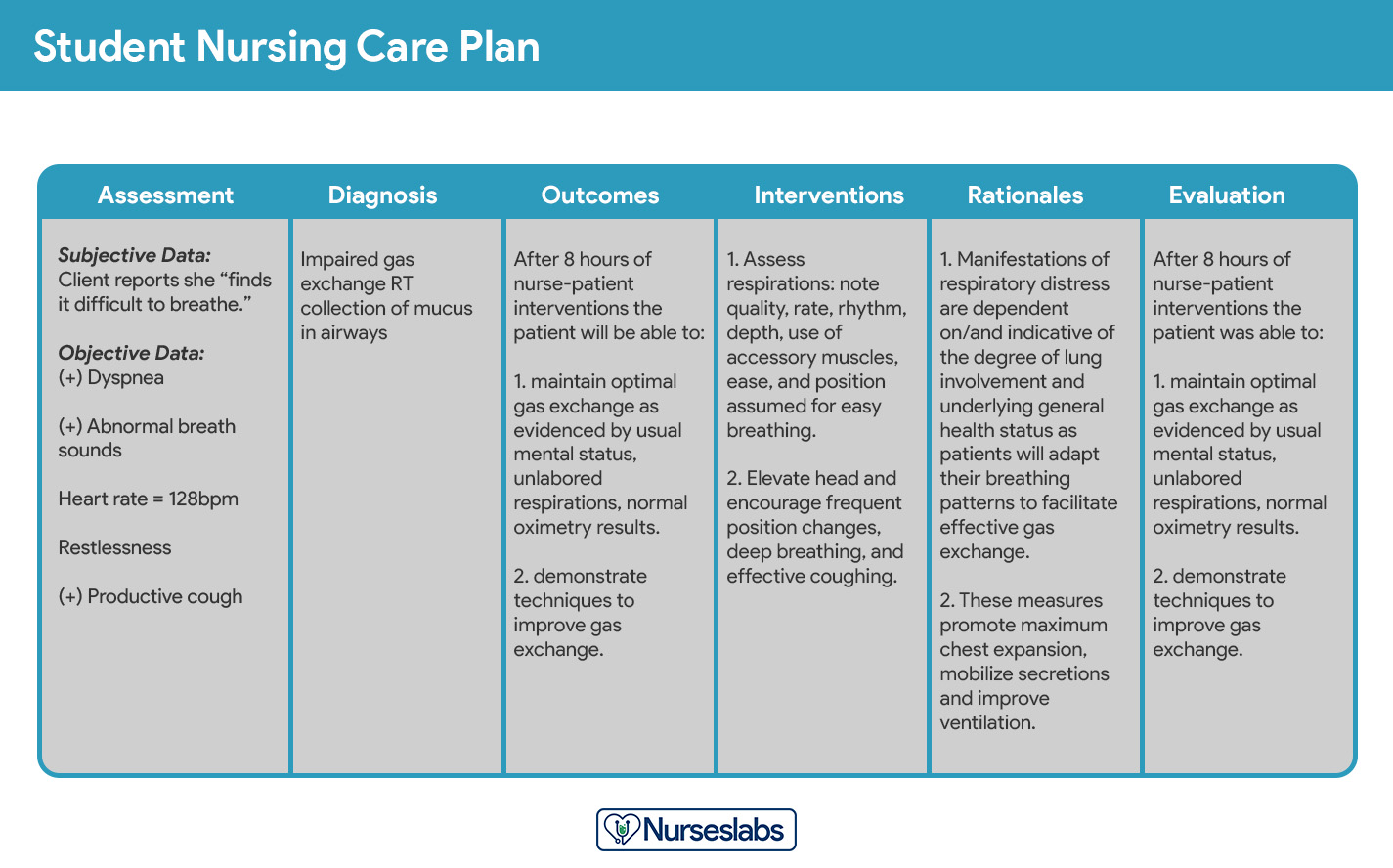
Student Care Plans
Student care plans are more lengthy and detailed than care plans used by working nurses because they serve as a learning activity for the student nurse.
Care plans by student nurses are usually required to be handwritten and have an additional column for “Rationale” or “Scientific Explanation” after the nursing interventions column. Rationales are scientific principles that explain the reasons for selecting a particular nursing intervention.
Writing a Nursing Care Plan
How do you write a nursing care plan (NCP)? Just follow the steps below to develop a care plan for your client.
Step 1: Data Collection or Assessment
The first step in writing a nursing care plan is to create a client database using assessment techniques and data collection methods (physical assessment, health history, interview, medical records review, and diagnostic studies). A client database includes all the health information gathered. In this step, the nurse can identify the related or risk factors and defining characteristics that can be used to formulate a nursing diagnosis. Some agencies or nursing schools have specific assessment formats you can use.
Critical thinking is key in patient assessment, integrating knowledge across sciences and professional guidelines to inform evaluations. This process, crucial for complex clinical decision-making, aims to identify patients’ healthcare needs effectively, leveraging a supportive environment and reliable information
Step 2: Data Analysis and Organization
Now that you have information about the client’s health, analyze, cluster, and organize the data to formulate your nursing diagnosis, priorities, and desired outcomes.
Step 3: Formulating Your Nursing Diagnoses
Nursing diagnoses are a uniform way of identifying, focusing on and dealing with specific client needs and responses to actual and high-risk problems. Actual or potential health problems that can be prevented or resolved by independent nursing intervention are termed nursing diagnoses.
We’ve detailed the steps on how to formulate your nursing diagnoses in this guide: Nursing Diagnosis (NDx): Complete Guide and List.
Step 4: Setting Priorities
Setting priorities involves establishing a preferential sequence for addressing nursing diagnoses and interventions. In this step, the nurse and the client begin planning which of the identified problems requires attention first. Diagnoses can be ranked and grouped as having a high, medium, or low priority. Life-threatening problems should be given high priority.
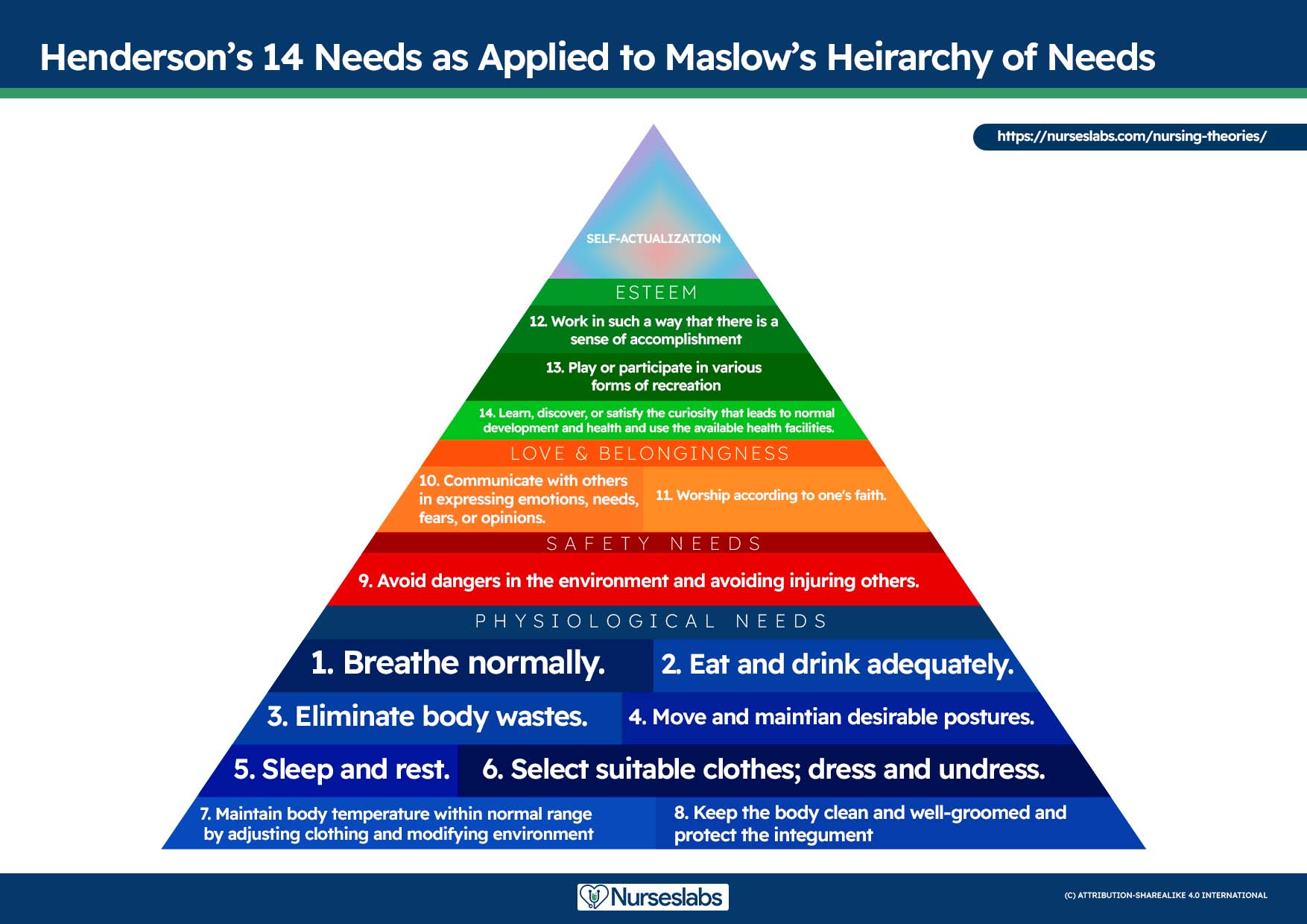
A nursing diagnosis encompasses Maslow’s Hierarchy of Needs and helps to prioritize and plan care based on patient-centered outcomes. In 1943, Abraham Maslow developed a hierarchy based on basic fundamental needs innate to all individuals. Basic physiological needs/goals must be met before higher needs/goals can be achieved, such as self-esteem and self-actualization. Physiological and safety needs are the basis for implementing nursing care and interventions. Thus, they are at the base of Maslow’s pyramid, laying the foundation for physical and emotional health.
Maslow’s Hierarchy of Needs
- Basic Physiological Needs: Nutrition (water and food), elimination (Toileting), airway (suction)-breathing (oxygen)-circulation (pulse, cardiac monitor, blood pressure) (ABCs), sleep, sex, shelter, and exercise.
- Safety and Security: Injury prevention (side rails, call lights, hand hygiene, isolation, suicide precautions, fall precautions, car seats, helmets, seat belts), fostering a climate of trust and safety (therapeutic relationship), patient education (modifiable risk factors for stroke, heart disease).
- Love and Belonging: Foster supportive relationships, methods to avoid social isolation (bullying), employ active listening techniques, therapeutic communication, and sexual intimacy.
- Self-Esteem: Acceptance in the community, workforce, personal achievement, sense of control or empowerment, accepting one’s physical appearance or body habitus.
- Self-Actualization: Empowering environment, spiritual growth, ability to recognize the point of view of others, reaching one’s maximum potential.
The client’s health values and beliefs, priorities, resources available, and urgency are factors the nurse must consider when assigning priorities. Involve the client in the process to enhance cooperation.
Step 5: Establishing Client Goals and Desired Outcomes
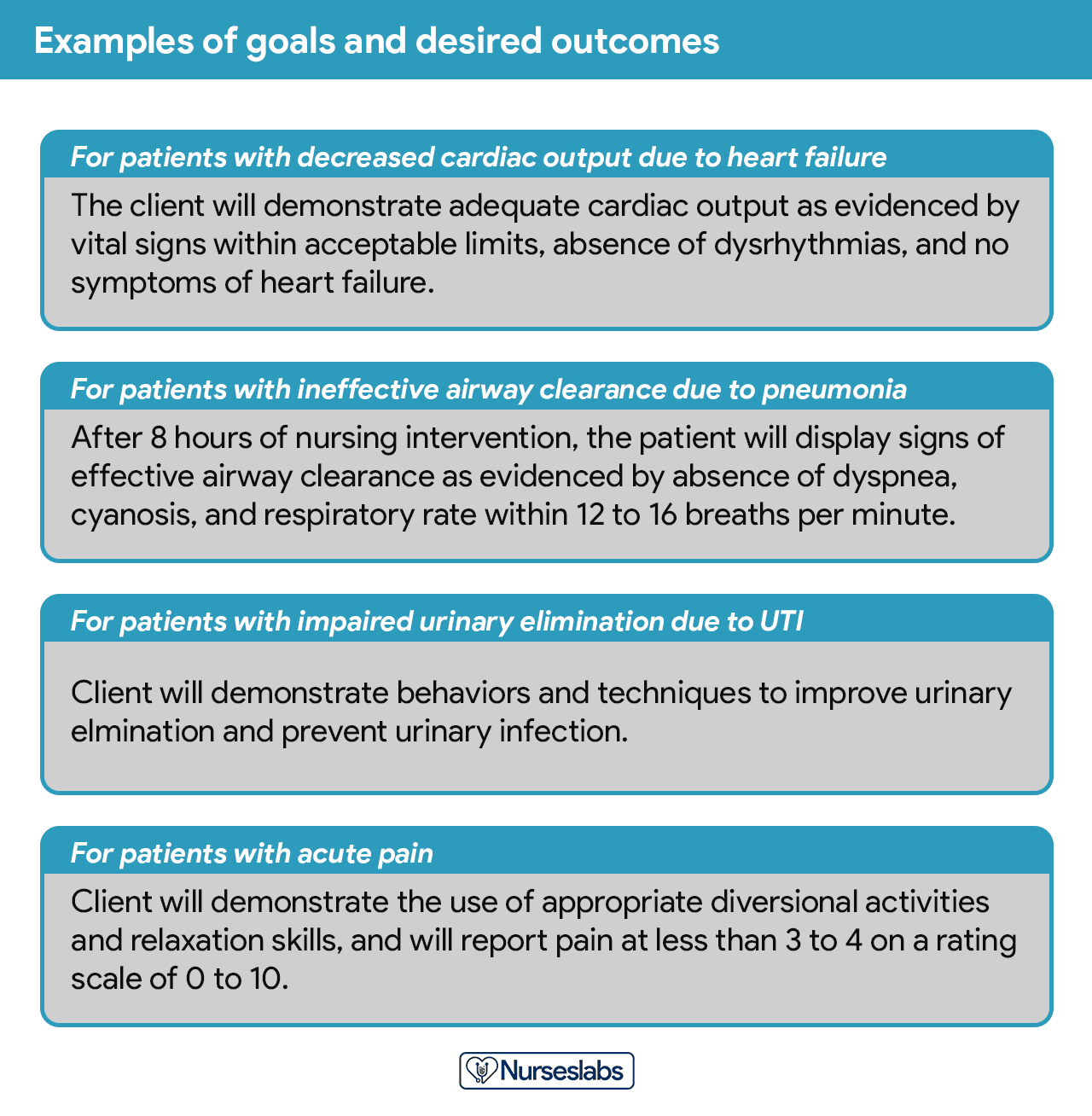
After assigning priorities for your nursing diagnosis, the nurse and the client set goals for each determined priority. Goals or desired outcomes describe what the nurse hopes to achieve by implementing the nursing interventions derived from the client’s nursing diagnoses. Goals provide direction for planning interventions, serve as criteria for evaluating client progress, enable the client and nurse to determine which problems have been resolved, and help motivate the client and nurse by providing a sense of achievement.
One overall goal is determined for each nursing diagnosis. The terms “goal outcomes“ and “expected outcomes” are often used interchangeably.
According to Hamilton and Price (2013), goals should be SMART. SMART stands for specific, measurable, attainable, realistic, and time-oriented goals.
- Specific. It should be clear, significant, and sensible for a goal to be effective.
- Measurable or Meaningful. Making sure a goal is measurable makes it easier to monitor progress and know when it reaches the desired result.
- Attainable or Action-Oriented. Goals should be flexible but remain possible.
- Realistic or Results-Oriented. This is important to look forward to effective and successful outcomes by keeping in mind the available resources at hand.
- Timely or Time-Oriented. Every goal needs a designated time parameter, a deadline to focus on, and something to work toward.
Hogston (2011) suggests using the REEPIG standards to ensure that care is of the highest standards. By this means, nursing care plans should be:
- Realistic. Given available resources.
- Explicitly stated. Be clear about precisely what must be done, so there is no room for misinterpretation of instructions.
- Evidence-based. That there is research that supports what is being proposed.
- Prioritized. The most urgent problems are being dealt with first.
- Involve. Involve both the patient and other members of the multidisciplinary team who are going to be involved in implementing the care.
- Goal-centered. That the care planned will meet and achieve the goal set.
Short-Term and Long-Term Goals
Goals and expected outcomes must be measurable and client-centered. Goals are constructed by focusing on problem prevention, resolution, and rehabilitation. Goals can be short-term or long-term. Most goals are short-term in an acute care setting since much of the nurse’s time is spent on the client’s immediate needs. Long-term goals are often used for clients who have chronic health problems or live at home, in nursing homes, or in extended-care facilities.
- Short-term goal. A statement distinguishing a shift in behavior that can be completed immediately, usually within a few hours or days.
- Long-term goal. Indicates an objective to be completed over a longer period, usually weeks or months.
- Discharge planning. Involves naming long-term goals, therefore promoting continued restorative care and problem resolution through home health, physical therapy, or various other referral sources.
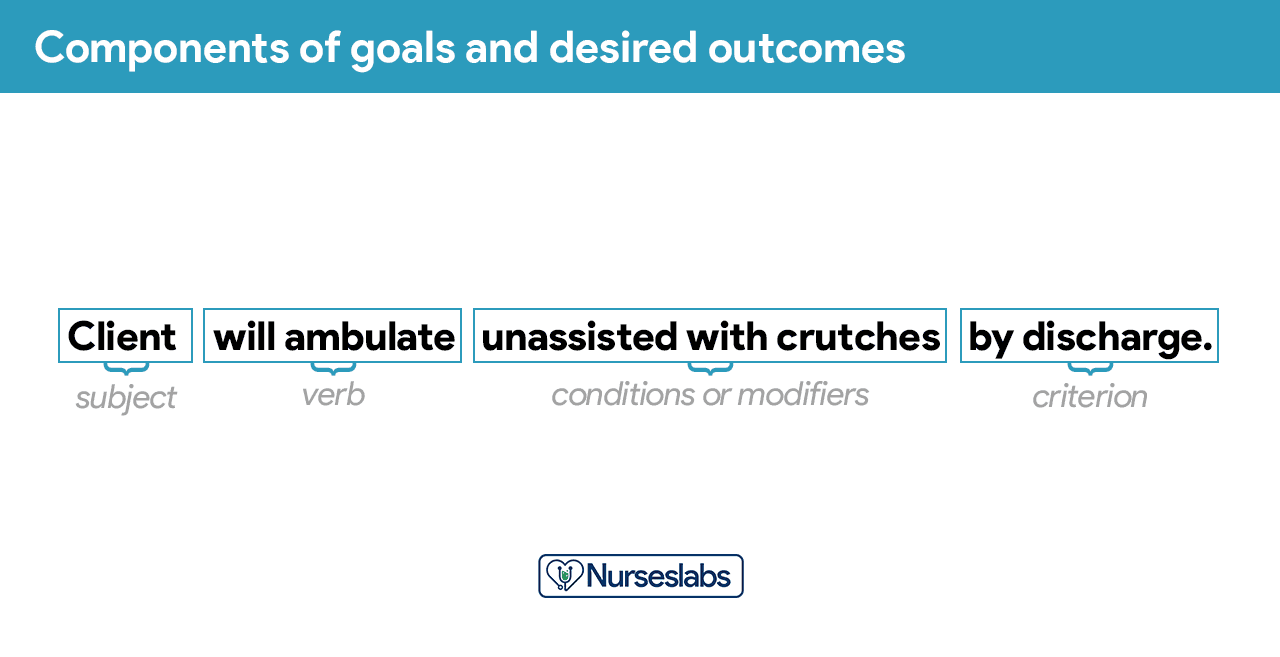
Components of Goals and Desired Outcomes
Goals or desired outcome statements usually have four components: a subject, a verb, conditions or modifiers, and a criterion of desired performance.
- Subject. The subject is the client, any part of the client, or some attribute of the client (i.e., pulse, temperature, urinary output). That subject is often omitted in writing goals because it is assumed that the subject is the client unless indicated otherwise (family, significant other).
- Verb. The verb specifies an action the client is to perform, for example, what the client is to do, learn, or experience.
- Conditions or modifiers. These are the “what, when, where, or how” that are added to the verb to explain the circumstances under which the behavior is to be performed.
- Criterion of desired performance. The criterion indicates the standard by which a performance is evaluated or the level at which the client will perform the specified behavior. These are optional.
When writing goals and desired outcomes, the nurse should follow these tips:
- Write goals and outcomes in terms of client responses and not as activities of the nurse. Begin each goal with “Client will […]” help focus the goal on client behavior and responses.
- Avoid writing goals on what the nurse hopes to accomplish, and focus on what the client will do.
- Use observable, measurable terms for outcomes. Avoid using vague words that require interpretation or judgment of the observer.
- Desired outcomes should be realistic for the client’s resources, capabilities, limitations, and on the designated time span of care.
- Ensure that goals are compatible with the therapies of other professionals.
- Ensure that each goal is derived from only one nursing diagnosis. Keeping it this way facilitates evaluation of care by ensuring that planned nursing interventions are clearly related to the diagnosis set.
- Care plans must be updated continually, not just at admission or discharge.
- Lastly, make sure that the client considers the goals important and values them to ensure cooperation.
Step 6: Selecting Nursing Interventions
Nursing interventions are activities or actions that a nurse performs to achieve client goals. Interventions chosen should focus on eliminating or reducing the etiology of the priority nursing problem or diagnosis. As for risk nursing problems, interventions should focus on reducing the client’s risk factors. In this step, nursing interventions are identified and written during the planning step of the nursing process; however, they are actually performed during the implementation step.
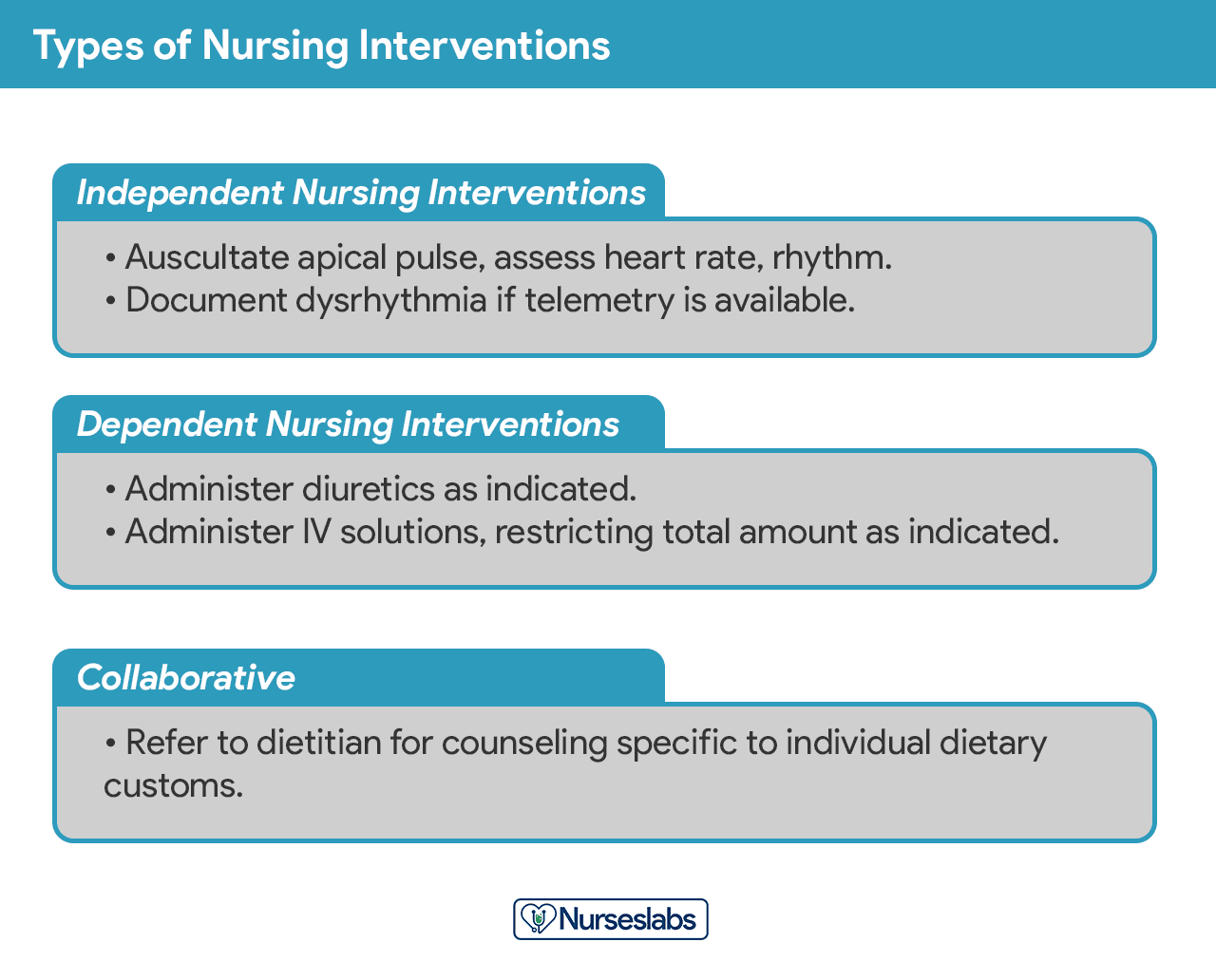
Types of Nursing Interventions
Nursing interventions can be independent, dependent, or collaborative:
- Independent nursing interventions are activities that nurses are licensed to initiate based on their sound judgement and skills. Includes: ongoing assessment, emotional support, providing comfort, teaching, physical care, and making referrals to other health care professionals.
- Dependent nursing interventions are activities carried out under the physician’s orders or supervision. Includes orders to direct the nurse to provide medications, intravenous therapy, diagnostic tests, treatments, diet, and activity or rest. Assessment and providing explanation while administering medical orders are also part of the dependent nursing interventions.
- Collaborative interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, dietitians, and therapists. These actions are developed in consultation with other health care professionals to gain their professional viewpoint.
Nursing interventions should be:
- Safe and appropriate for the client’s age, health, and condition.
- Achievable with the resources and time available.
- Inline with the client’s values, culture, and beliefs.
- Inline with other therapies.
- Based on nursing knowledge and experience or knowledge from relevant sciences.
When writing nursing interventions, follow these tips:
- Write the date and sign the plan. The date the plan is written is essential for evaluation, review, and future planning. The nurse’s signature demonstrates accountability.
- Nursing interventions should be specific and clearly stated, beginning with an action verb indicating what the nurse is expected to do. Action verb starts the intervention and must be precise. Qualifiers of how, when, where, time, frequency, and amount provide the content of the planned activity. For example: “Educate parents on how to take temperature and notify of any changes,” or “Assess urine for color, amount, odor, and turbidity.”
- Use only abbreviations accepted by the institution.
Evidenced-Based Practice
When selecting nursing interventions, it’s best to draw from published clinical practice guidelines (CPGs) or consensus statements that address the patient’s specific diagnosis. For example, if you’re caring for someone with heart failure, you might reference American Heart Association guidelines that recommend daily weight checks, a reduced-sodium diet, and careful monitoring of fluid intake. If you’re treating a patient with diabetes, check the American Diabetes Association guidelines for interventions such as regular blood glucose testing, foot care routines, and scheduling meals with medication times.
Step 7: Providing Rationale
Rationales, also known as scientific explanations, explain why the nursing intervention was chosen for the NCP.
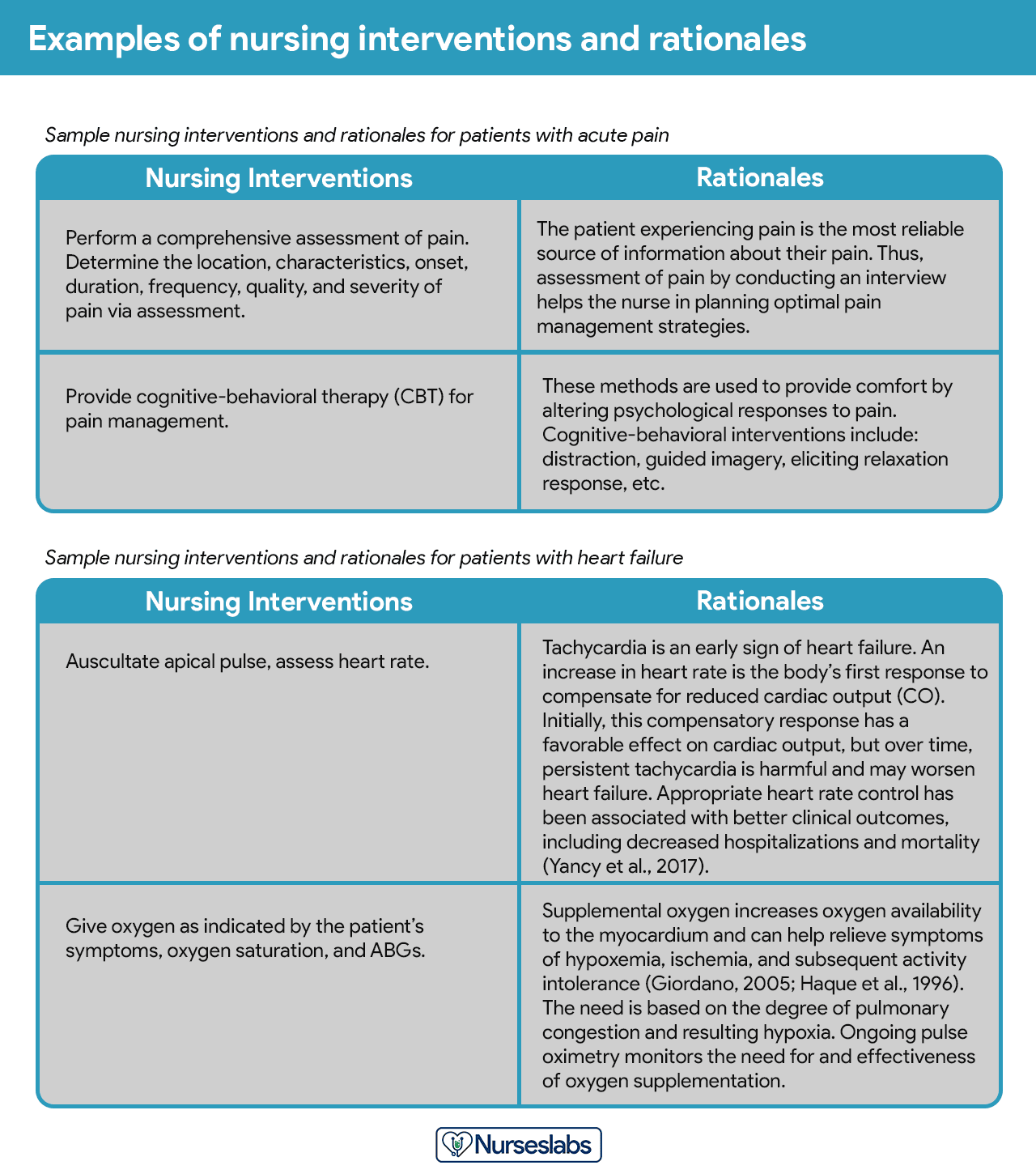
Rationales do not appear in regular care plans. They are included to assist nursing students in associating the pathophysiological and psychological principles with the selected nursing intervention.
Step 8: Evaluation
Evaluation is a planned, ongoing, purposeful activity in which the client’s progress towards achieving goals or desired outcomes is assessed, and the effectiveness of the nursing care plan (NCP). Evaluation is an essential aspect of the nursing process because the conclusions drawn from this step determine whether the nursing intervention should be terminated, continued, or changed.
Step 9: Putting it on Paper
The client’s care plan is documented according to hospital policy and becomes part of the client’s permanent medical record, which may be reviewed by the oncoming nurse. Different nursing programs have different care plan formats. Most are designed so that the student systematically proceeds through the interrelated steps of the nursing process, and many use a five-column format.
Nursing Care Plan List
This section lists the sample nursing care plans (NCP) and nursing diagnoses for various diseases and health conditions. They are segmented into categories:
Basic Nursing and General Care Plans
Miscellaneous nursing care plans examples that don’t fit other categories:
Surgery and Perioperative Care Plans
Care plans that involve surgical intervention.
Cardiac Care Plans
Nursing care plans about the different diseases of the cardiovascular system:
Endocrine and Metabolic Care Plans
Nursing care plans (NCP) related to the endocrine system and metabolism:
| Acid-Base Imbalances |
|---|
| Metabolic Acidosis |
| Metabolic Alkalosis |
| Respiratory Acidosis |
| Respiratory Alkalosis |
Gastrointestinal
Care plans (NCP) covering the disorders of the gastrointestinal and digestive system:
Hematologic and Lymphatic
Care plans related to the hematologic and lymphatic system:
Infectious Diseases
NCPs for communicable and infectious diseases:
Integumentary
All about disorders and conditions affecting the integumentary system:
| Integumentary Care Plans |
|---|
| Burn Injury |
| Dermatitis |
| Herpes Zoster (Shingles) |
| Pressure Ulcer (Bedsores) |
| Wound Care and Skin/Tissue Integrity |
Maternal and Newborn Care Plans
Nursing care plans about the care of the pregnant mother and her infant. See care plans for maternity and obstetric nursing:
Mental Health and Psychiatric
Care plans for mental health and psychiatric nursing:
Musculoskeletal
Care plans related to the musculoskeletal system:
Neurological
Nursing care plans (NCP) for related to nervous system disorders:
Ophthalmic
Care plans relating to eye disorders:
| Ophthalmic Care Plans |
|---|
| Cataracts |
| Glaucoma |
| Macular Degeneration |
Pediatric Nursing Care Plans
Nursing care plans (NCP) for pediatric conditions and diseases:
| Pediatric Nursing Care Plans |
|---|
| Child Abuse |
| Cleft Lip and Cleft Palate |
| Dying Child |
| Febrile Seizure |
| Hospitalized Child |
| Hydrocephalus |
| Otitis Media |
| Spina Bifida |
| Tonsillitis and Adenoiditis |
Reproductive
Care plans related to the reproductive and sexual function disorders:
| Reproductive Care Plans |
|---|
| Cryptorchidism (Undescended Testes) |
| Hysterectomy |
| Hypospadias and Epispadias |
| Mastectomy |
| Menopause |
| Prostatectomy |
Respiratory
Care plans for respiratory system disorders:
Urinary
Care plans related to the kidney and urinary system disorders:
Recommended Resources
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health
Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

References and Sources
Recommended reading materials and sources for this NCP guide:
- Björvell, C., Thorell-Ekstrand, I., & Wredling, R. (2000). Development of an audit instrument for nursing care plans in the patient record. BMJ Quality & Safety, 9(1), 6-13. [Link]
- DeLaune, S. C., & Ladner, P. K. (2011). Fundamentals of nursing: Standards and practice. Cengage learning.
- Freitas, F. A., & Leonard, L. J. (2011). Maslow’s hierarchy of needs and student academic success. Teaching and learning in Nursing, 6(1), 9-13.
- Hamilton, P., & Price, T. (2007). The nursing process, holistic. Foundations of Nursing Practice E-Book: Fundamentals of Holistic Care, 349.
- Lee, T. T. (2004). Evaluation of computerized nursing care plan: instrument development. Journal of Professional Nursing, 20(4), 230-238.
- Lee, T. T. (2006). Nurses’ perceptions of their documentation experiences in a computerized nursing care planning system. Journal of Clinical Nursing, 15(11), 1376-1382.
- Rn, B. O. C., Rn, H. M., Rn, D. T., & Rn, F. E. (2000). Documenting and communicating patient care: Are nursing care plans redundant?. International Journal of Nursing Practice, 6(5), 276-280.
- Stonehouse, D. (2017). Understanding the nursing process. British Journal of Healthcare Assistants, 11(8), 388-391.
- Yildirim, B., & Ozkahraman, S. (2011). Critical thinking in nursing process and education. International journal of humanities and social science, 1(13), 257-262.




























Leave a Comment